Effects of bilateral discectomy and bilateral discopexy on black Merino sheep rumination kinematics: TEMPOJIMS — phase 1 — pilot blinded, randomized preclinical study
Abstract
Background: The temporomandibular joint interposal study (TEMPOJIMS) is a rigorous preclinical trial divided in 2 phases. In phase 1 the authors investigated the role of the TMJ disc and in phase 2 the authors evaluated 3 different interposal materials. The present work of TEMPOJIMS - phase 1, investigated the effects of bilateral discectomy and discopexy in sheep mastication and rumination.
Methods: This randomized, blinded and controlled preclinical trial (in line with the ARRIVE guidelines) was conducted in 9 Black Merino sheep to evaluate changes in mastication and rumination after bilateral discectomy and bilateral discopexy, by comparing with a sham surgery control group. The outcomes evaluated were: (1) absolute masticatory time; (2) ruminant time per cycle; (3) ruminant kinematics, and (4) ruminant area. After baseline evaluation and surgical interventions, the outcomes were recorded over 3 successive days, every 30 days, for 6 months.
Results: The first month after intervention seemed to be the critical period for significant kinematic changes in the discectomy and discopexy groups. However, 6 months after the bilateral interventions, no significant changes were noticed when compared with the control group.
Conclusions: In this study, bilateral discectomy and discopexy had no significant effect in mastication and ruminatory movement. The introduction of kinematic evaluation presents a new challenge that may contribute to the improvement of future studies on the TMJ domain.
Introduction
The area of temporomandibular joint (TMJ) bioengineering is growing fast, and the potential for developing a TMJ interposal disc is immense. Rigorous preclinical trials are therefore needed for the normal progress of translational medicine. However, before using valuable resources and funds for TMJ bioengineering, it is important to improve our understanding of the effects induced at the temporomandibular joint by common surgical interventions.
TMJ discectomy is the most performed intracapsular surgery. With good overall results, this technique remains a reasonable choice for internal derangement not responding to nonsurgical treatment (Nyberg et al., 2004; Eriksson and Westesson, 2001;Mazzonetto and Spagnoli, 2001; Bjørnland and Larheim, 2003; Trumpy and Lyberg, 1995). Nevertheless, it still is a controversial technique because it does not restore structural or biological properties of the TMJ (Takaku et al., 2000). TMJ discopexy is a less invasive surgery technique used to restore ideal TMJ disc position, but with variable results (Sharma et al., 2010).
Despite the large number of discectomy and discopexy procedures performed annually, to the best of our knowledge there have been no randomized, blinded, controlled trials that have investigated, in human or animal, the jaw movement implications of bilateral discectomy and bilateral discopexy.
Small-size, mid-size, and large animal models have been used to investigate the histological effects of unilateral discectomy (Bjørnland and Haanaes, 1999; Dimitroulis and Slavin, 2006; Ogi et al., 1999; Sato et al., 2002; Tong and Tideman, 2000), leading to diverse results, from minor degenerative changes to TMJ ankylosis. This heterogeneous results are probably due to limitations regarding animal choice, study design, and the use of a unilateral approach with the contralateral side as a control, which may have induced bias in available results (Cohen et al., 2014).
As reported in a survey, commissioned by the National Centre for the Replacement, Refinement and Reduction of Animals in Research (NC3Rs) (Kilkenny et al., 2009), only 59% of the 271 randomly chosen articles assessed stated the hypothesis or objective of the study, and the number and characteristics of the animals used (i.e., species/strain, sex, and age/weight). Most of the papers surveyed did not report using randomization (87%) or blinding (86%) to reduce bias in animal selection and outcome assessment. Only 70% of the publications that used statistical methods fully described them and presented the results with a measure of precision or variability (Kilkenny et al., 2009). These findings are a cause for concern, and are consistent with reviews of many research areas, including clinical studies, published in recent years (Kilkenny et al., 2009; Sharma et al., 2010; Van der Worp et al., 2010). Furthermore, most of the previous studies have focused on histological and imaging differences, but additional inputs are essential to obtain a clear understanding of TMJ functionality.
In this paper the authors report, for the first time, on a high-quality, preclinical study that evaluates the impacts of bilateral discectomy and bilateral discopexy on mastication and rumination kinematics in black Merino sheep, in comparison with a sham surgery control group.
The evaluation of mastication and rumination kinematics of the sheep jaw was based on the normal processes used by ruminants to break down particulate dry matter: (1) initial chewing during eating and (2) further chewing during rumination (Pearce, 1967). The authors discriminated between the two processes and analyzed them separately. To analyze the initial chewing the authors examined the time taken to eat a dose of dry pellets, naming this outcome absolute masticatory time. With this outcome the authors expected to determine if TMJ surgical interventions could induce significant changes in the initial chewing time. To analyze the ruminant chewing phase, a special cage was created and 15 ruminant chewing cycles were recorded with a video camera. Using Foundry Nuke (2D tracking) and Image J software, ruminant movements in the frontal plane were analyzed to obtain: (1) rumination time per cycle, (2) rumination kinematics, and (3) rumination area.
The temporomandibular joint interposal material study (TEMPOJIMS) was planned with a rigorous design, in line with the ARRIVE guidelines (Kilkenny et al., 2009). A Randomized, preclinical study with blinded outcomes, was needed in this field in order to increase the quality of further TMJ studies, improve future treatment options for patients undergoing surgery for TMJ disc replacement, and facilitate interpretation of future studies regarding TMJ interposal materials using TEMPOJIMS design.
Materials and methods
TEMPOJIMS study was a preclinical study divided into two phases (Ângelo et al., 2017). This paper focuses on the kinematic outcomes of phase 1, aiming to understand the impact of TMJ bilateral discectomy versus TMJ bilateral discopexy, in comparison with a sham surgery control group, on black Merino sheep.
Study design
The rationale and protocol for the TEMPOJIMS preclinical trial are publicly available (Ângelo et al., 2017).
Study population and sample
A variety of strains/breeds of sheep have been used in previous TMJ investigations. To reduce biological variability, the authors performed this study in a black Merino sheep strain (Angelo et al., 2016). In phase 1 the authors used 10 black Merino sheep with the following inclusion criteria: certified black Merino sheep, adult (aged between 2 and 5 years), female, good health condition (veterinary checks were performed on all animals), and normal dentition (with 32 teethd8 mandibular incisors, 12 premolars, and 12 molars).
Randomization
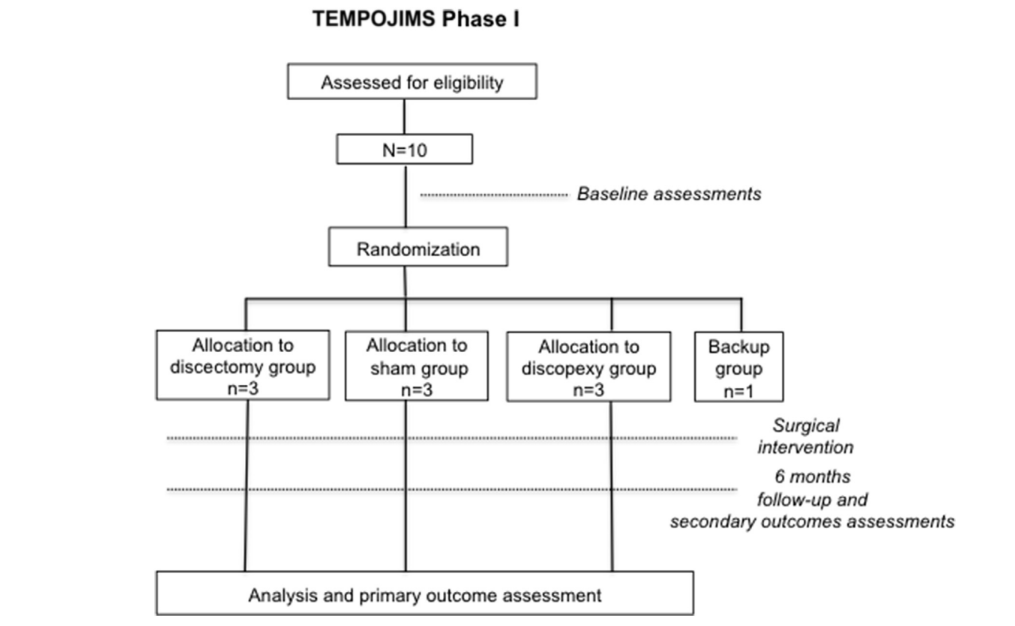
The randomization process was performed by a statistical team not involved in the outcome assessments. Ten sheep were randomly allocated to intervention groups as follows: bilateral discectomy group (n = 3), bilateral discopexy group (n = 3), sham surgery group (n = 3), and back-up group (n = 1). The one back-up sheep was in case of death occurring as a result of anesthesia or other complications not related to surgical intervention. The allocation to each randomized group was performed preoperatively using sealed envelopes (Fig. 1).
Procedures
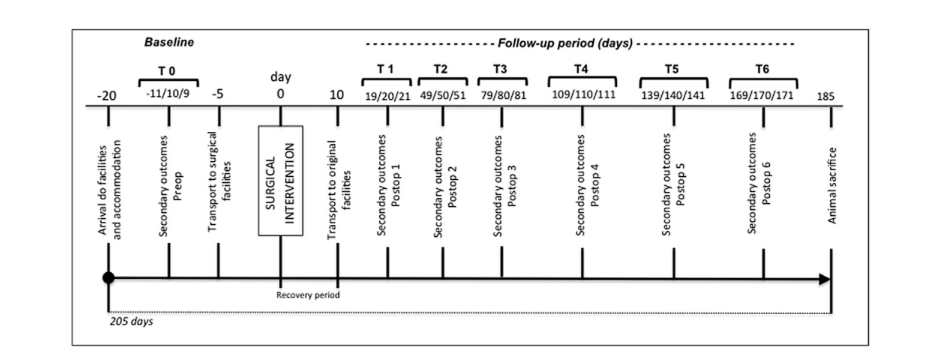
Ten eligible sheep were assigned to their baseline pilot secondary outcomes, measured at days 11, 10, and 9 before surgery in TEMPOJIMS facilities (Fig. 2). Transportation to surgical facilities occurred 5 days before surgery to avoid animal stress and allow familiarization with temporary accommodation. The surgical team was not blinded to treatment allocation, given the type of intervention; however, the surgical team members were not involved in outcome assessment. Serious adverse events were defined as events that were fatal or that resulted in life-threatening or persistent disability, more than 10% weight loss per week, or clinically significant hazards/harm to the animal.
Anesthesia protocol
Fasting and water restriction were required 24 h before surgery. Sedation was performed with diazepam (0.5 mg/kg IV), followed by anesthesia induction with ketamine (5 mg/kg IV). Oral intubation was performed and anesthesia was maintained with isoflurane (1.5e2%). To assure animal analgesia, Meloxicam (0.5 mg/kg IV/bid) was administered on the surgery day and over the following 4 days. Antibiotic prophylaxis with amoxicillin and clavulanic acid was administrated for 5 days.
Surgical intervention
(A) Bilateral discectomy group (n = 3): during general anesthesia, the surgical team performed a preauricular incision and a blunt dissection of the soft tissue covering the joint. The joint area was disclosed and the articular capsule was incised. The disc and its attachments were identified. The medial, anterior, posterior, and lateral disc attachments were detached and discectomy was performed. The wound was closed in layers with Vicryl 3/0.
(B) Bilateral discopexy group (n = 3): during general anesthesia, the surgical team performed a preauricular incision and a blunt dissection of the soft tissue covering the joint. The joint area was disclosed and the articular capsule was incised. The disc and its attachments were identified. The lateral and posterior disc attachments were detached and sutured with PDS 3/0. The wound was closed in layers with Vicryl 3/0.
(С) Sham surgery group (n = 3): during general anesthesia, the surgical team performed a preauricular incision and a blunt dissection of the soft tissue covering the joint. The TMJ articular capsule was not incised. The wound was closed in layers with Vicryl 3/0.
Follow-up assessments
Baseline assessment (T0) was performed before surgery on days —11, —10, and —9 (Table 1). Ten days after surgery, animals were transported to TEMPOJIMS facilities. Follow-up recording of outcomes began on days 19, 20, and 21 after surgery (T1) and was repeated every 30 days for 6 months (Fig. 2). T0eT6 were based on the means of the three measurements. The assessments were performed by two specially trained assessors who were not affiliated with the interventions. All animals had bilateral scars to reduce possible bias.
Kinematic outcomes
Kinematic outcomes evaluated were: (1) absolute masticatory time; (2) ruminatory time per cycle; (3) ruminatory kinematics; and (4) ruminatory area.
To measure the referred outcomes, a specific cage was built with a frontal window and a feeder. All assessments were performed by researchers blinded to surgical intervention, and were designed to evaluate masticatory time changes and to ruminatory kinematics. These outcomes were as follows:
- Absolute masticatory time: based on the assessment timetable (Fig. 2), at 9:00 am the 10 sheep were placed in their individual cages. A dose of 150 g of dry pellets (Rico Gado A3) was introduced in the feeder and the time taken to eat all the pellets was measured with a chronometer.
- Ruminatory time per cycle: based on the assessment timetable (Fig. 2), we recorded 15 ruminant cycles approximately 4 h after the 150g feed. We used a Canon 7D video camera to record images at 25 frames per second. The number of frames per cycle was then divided by 25 to obtain time in seconds per cycle.
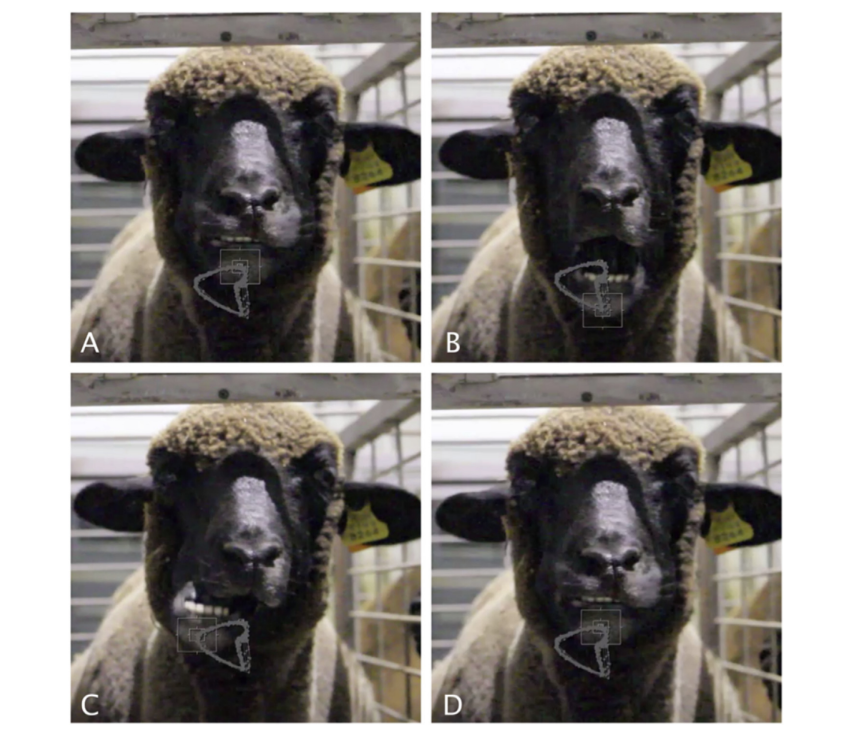
- Ruminatory kinematics: we used Foundry Nuke (2D tracking) software to track jaw movements and calculate the average ruminant cycle. Using After Effects software, we converted the 2D tracking into a geometric form.
- Ruminatory area: we determined an average for 15 cycles, and created a geometric representation. Using the software Image J, we performed a quantitative measurement, in pixels, of the average ruminatory area.
Statistical analysis
The TEMPOJIMS phase 1 randomized, controlled, preclinical trial used ten black Merino sheep, with a 6-month follow-up. The primary analysis tested the effects of the independent variable (IV)
for three experimental conditions: 1 = bilateral discectomy; 2 = bilateral discopexy; 3 = sham surgery, using a series of pre-tests (T0) and post-tests (T1 to T6). The dependent variables (outcome
measures) were: the time to eat 150 g of pellets; the ruminant time per cycle; and the ruminant area. These events were measured three times in the pre-tests to promote invariance in the outcome measures before surgical intervention (IV). The secondary tests (post-tests) analyzed the outcomes using three measurements, at six time intervals (T1 to T6), at the same place, and hour as the pre- tests (Fig. 2).
All statistical analyses were performed using the Statistical Package for Social Sciences (IBM SPSS, version 22.0). ShapiroeWilk tests were performed for pre-tests (T0) and post-tests (T1 to T6), showing a normal distribution in all groups for all tests (p > 0.05), except for T4 and T6 rumination areas for discopexy (ShapiroeWilk = 0.761 and 0.384; p < 0.05).
Additionally, Levene statistics were performed to test the homogeneity of variances. Statistically significant results were found at T1, T2, and T5 for rumination area (Levene statistics = 8.59, 6.35, and 7.82; p < 0.05), which led to non-parametric tests being calculated for these times. For the pre-tests and other time groups, variances were homogeneous (p > 0.07), leading to parametric tests.
A one-way analysis of variance (ANOVA) (or the non-parametric equivalent KruskaleWallis test) was performed for cross-sectional analysis to compare the outcome variables at the three levels of the IV before and after the random treatment group assignment. Fisher LSD and Games-Howell Post-hoc tests were performed for equal variances assumed and not assumed, respectively. For longitudinal analysis, Mauchly's test of sphericity was non-significant for absolute masticatory time (Mauchly's W = 0.004; p = 0.589), allowing a parametric one-way ANOVA test with repeated measures, taking as within-subject effects observations before (T0) and after (T1 to T6) surgery for bilateral discectomy, bilateral discopexy, and sham surgery conditions. For rumination area, a Greenhouse- Geisser corrected test was used, due to a Mauchly's W value of 0.000; p = 0.011.
Results
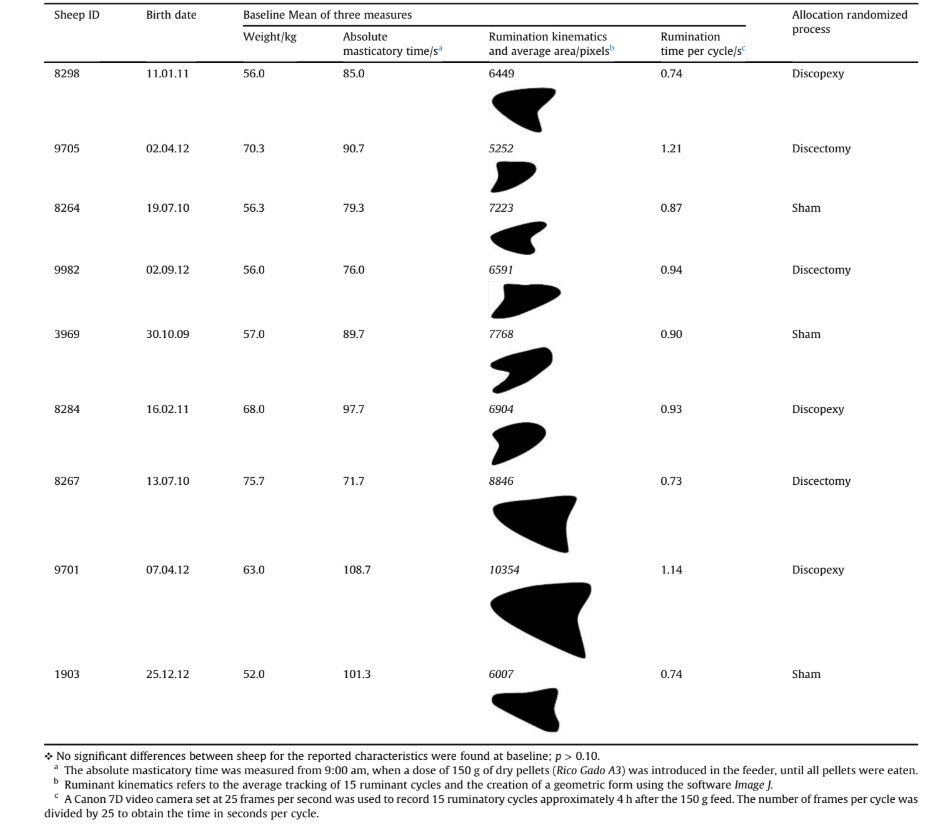
Descriptive baseline statistics are presented in Table 1. Four outcomes were analyzed: (1) absolute masticatory time; (2) ruminatory time per cycle; (3) ruminatory kinematics; and (4) ruminatory area.
1) Absolute masticatory time
Cross-sectional analysis: The authors compared the absolute masticatory times for the three groups each month, post-surgery (T1 to T6). A one-way ANOVA (or the non-parametric equivalent KruskaleWallis test) was performed, showing significant differences between the three groups only in T1-p = 0.03 (one-tailed), effect size of η2p = 0.736 (1-β) = 0.804 (Table 2) due to the higher values for discopexy in comparison with sham surgery, as shown using a Games-Howell post-hoc test (p = 0.028). Throughout the baseline and the remaining follow-up period (T2-T6), no statistically significant differences were found between discectomy, discopexy, and sham surgery conditions (p > 0.20).
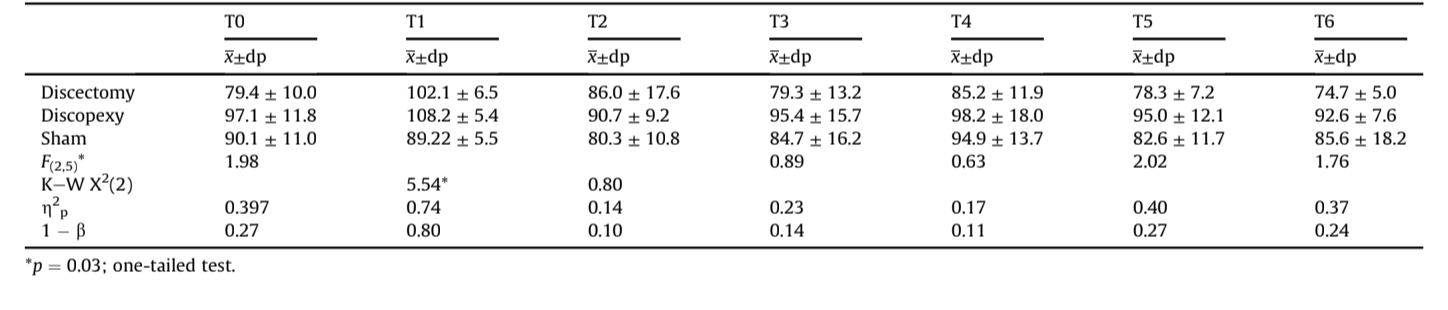
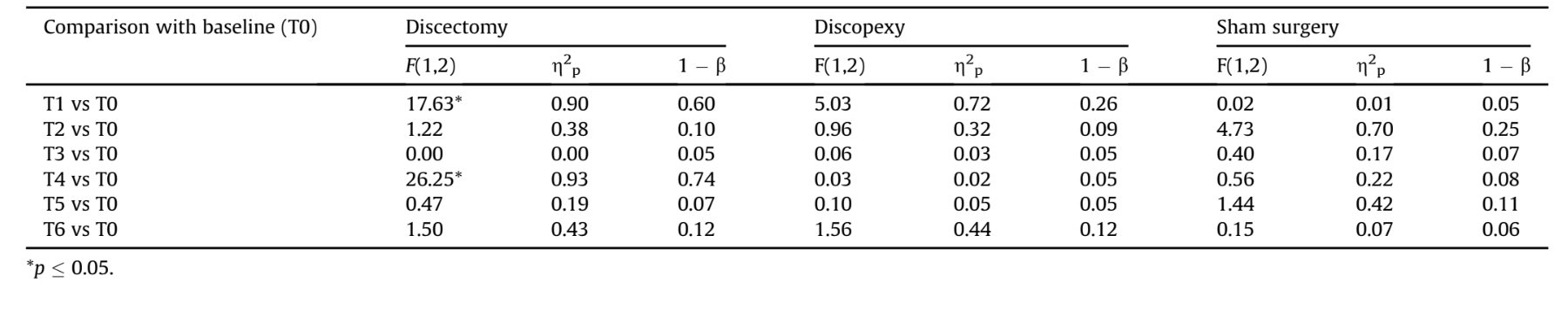
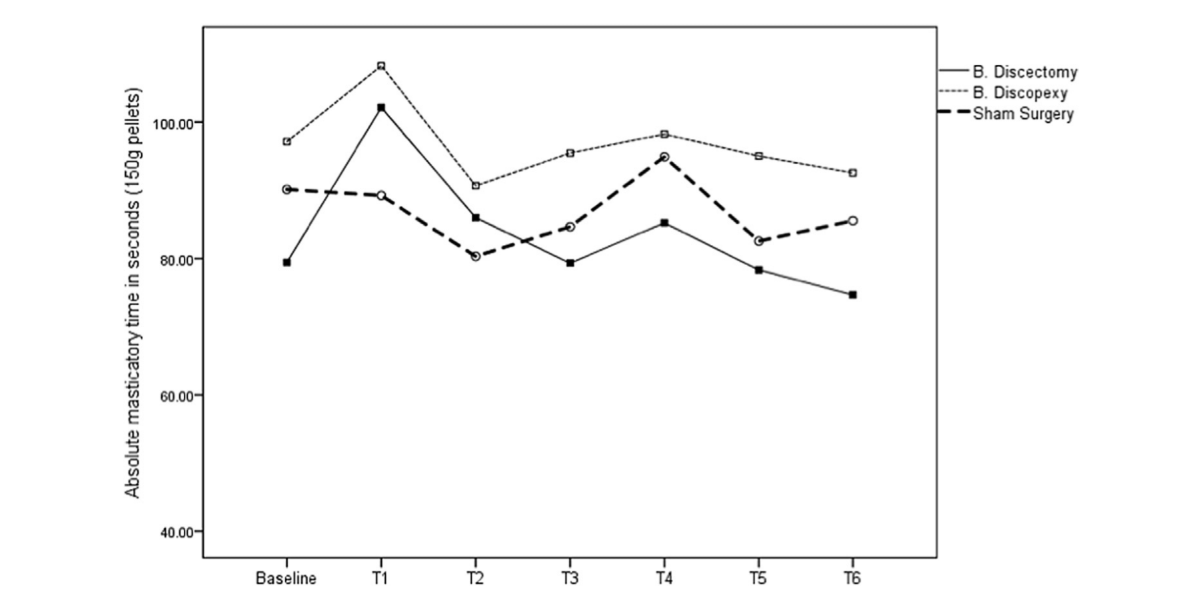
Longitudinal analysis: A one-way ANOVA with repeated measures was performed, taking as within-subject effects months before (T0) and after surgery (T1 to T6) for discectomy, discopexy, and sham surgery conditions. Significant effects across time were found for discectomy - F(6, 12) = 5.67, p = 0.005, η2p = 0.739 (1-β) = 0.947dbut not for discopexy and sham surgery - F(6, 12) = 2.65 and 1.59, p > 0.07, η2p = 0.570 and 0.443 (1-β) = 0.635 and 0.403, respectively. Considering the differences in relation to the baseline (Table 3), the within-subject contrasts identified a statistically significant increase only for discectomy between T0 and T1 (effect size of 90%; observed power of 0.60) and between T0 and T4 (effect size of 93%; observed power of 0.74). For discopexy and sham surgery, despite the effect sizes and considering the low observed powers, the differences in relation to the baseline were not statistically significant. Fig. 4 represents absolute masticatory time for the baseline and from T1 to T6.
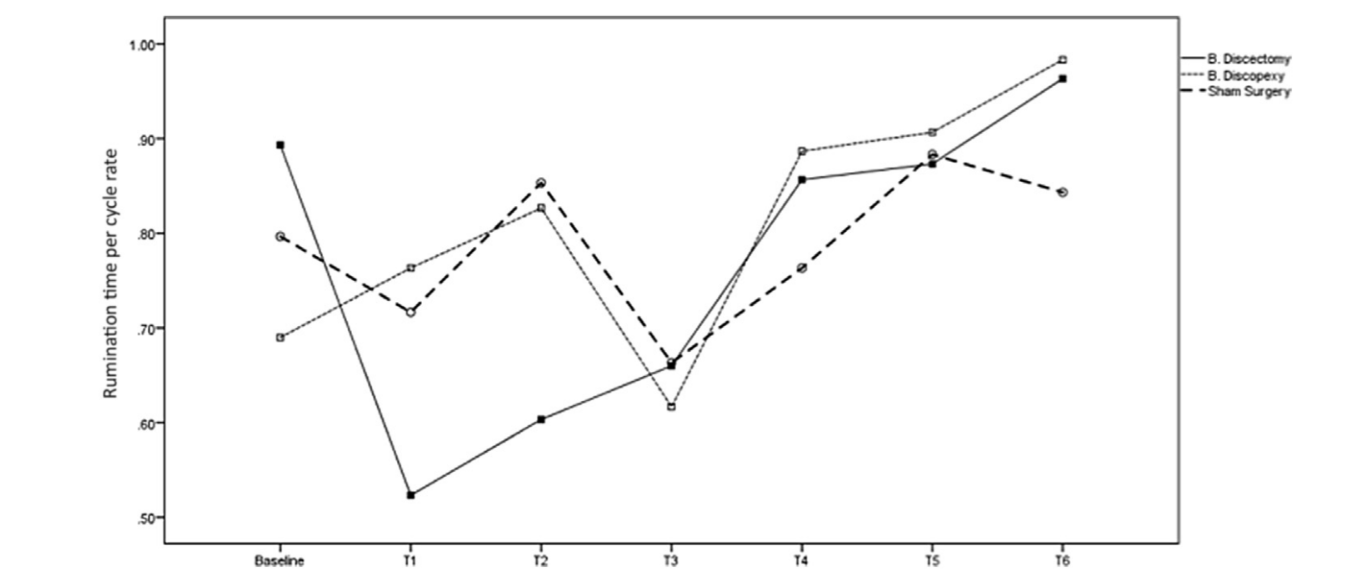
2) Rumination time per cycle
Cross-sectional analysis: Rumination time per cycle rate did not vary across groups both in the pre-test (T0) and in all times for the post-test (p > 0.20), as shown in Table 4.
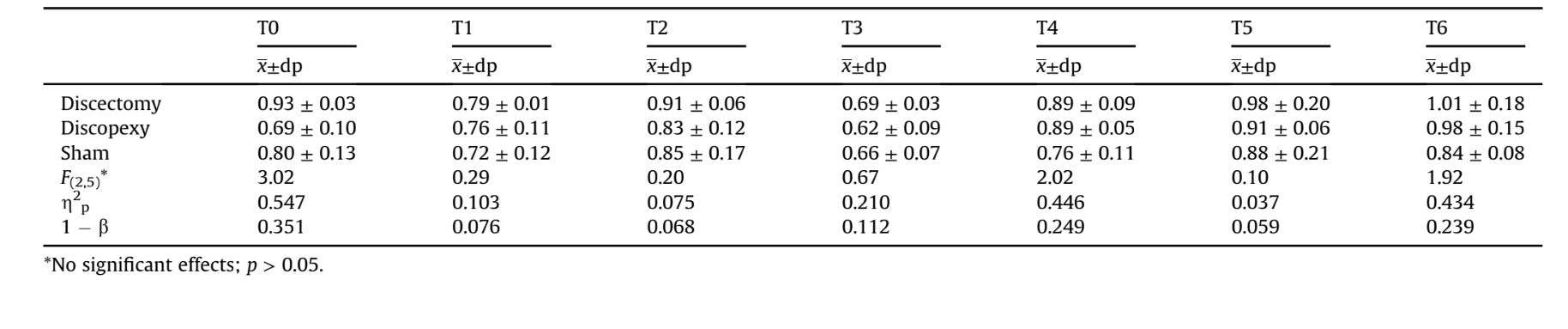
Longitudinal analysis: A one-way ANOVAwith repeated measures was performed, taking as within-subject effects the baseline and the 6 months after surgery for discectomy, discopexy, and sham surgery (see Table 5).
A significant effect across time was found for discopexy and sham surgery - F(6, 6) = 6.87 and 4.11, p < 0.018, η2p = 0.773 and 0.673 (1-β) = 0.977 and 0.845, respectively but not for discectomy - F(6, 6) = 2.70, p = 0.126, η2p = 0.730 (1-β) = 0.455.
The comparison of rumination time per cycle rate between the baseline and months after the surgery identified two differences for discopexy, (T5 vs. T0) with an acceptable power (effect size of 95%). For discectomy and sham surgery no significant differences were found in relation to baseline. Fig. 5 illustrates the rumination time per cycle rate in the baseline, and from T1 to T6. As can be seen, lower scores were obtained for times T1, T2, and T3, suggesting that sheep TMJ recovery started at T4.
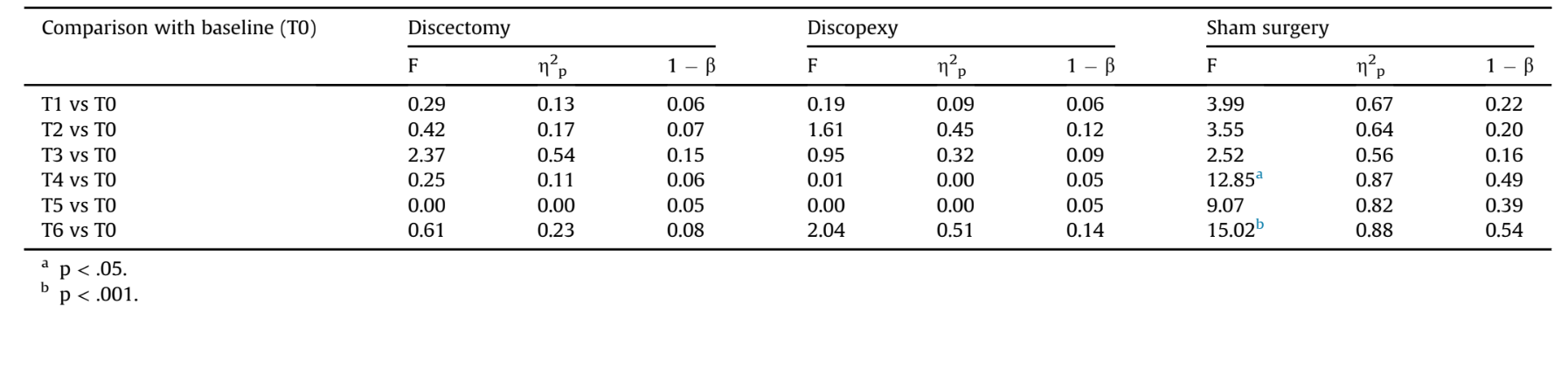
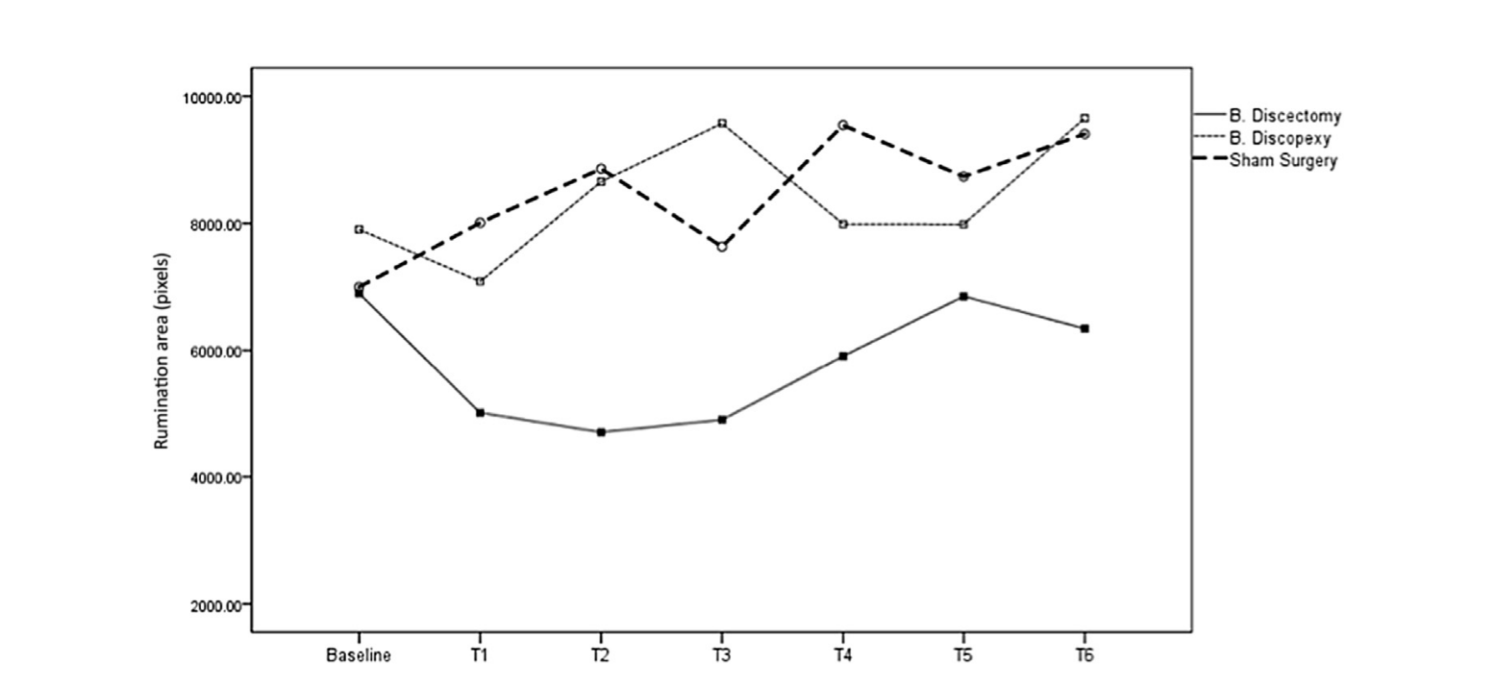
3) Ruminatory kinematics and area
Descriptive results for rumination kinematics and average area of rumination are presented in Fig. 6.
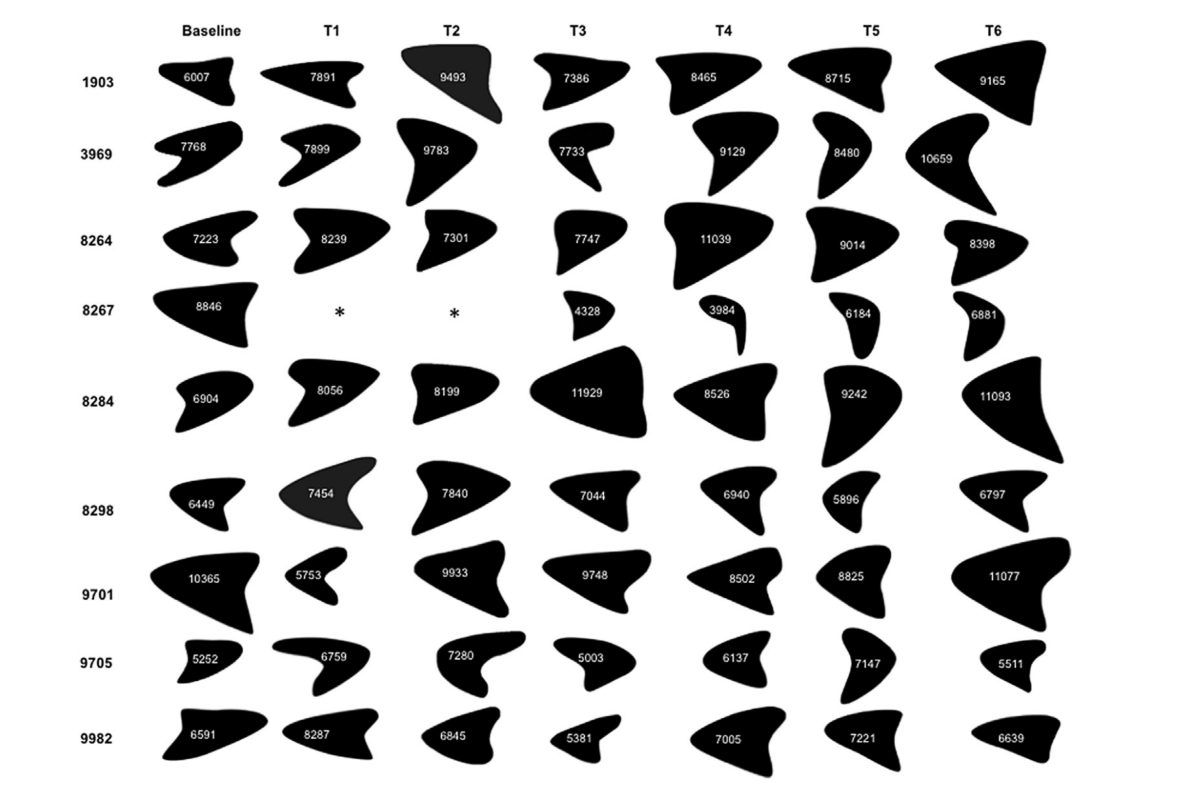
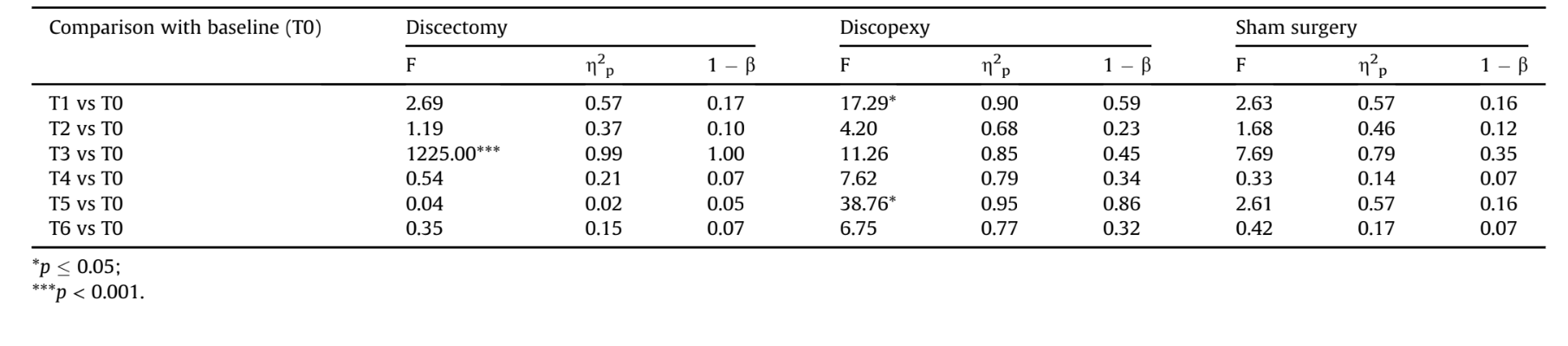
Cross-sectional analysis: Rumination areas only varied across groups in T3 and T4. For T3, the Fisher LSD post-hoc test identified a significant superiority for the discopexy area compared with the discectomy area (p = 0.008) (see Table 6).
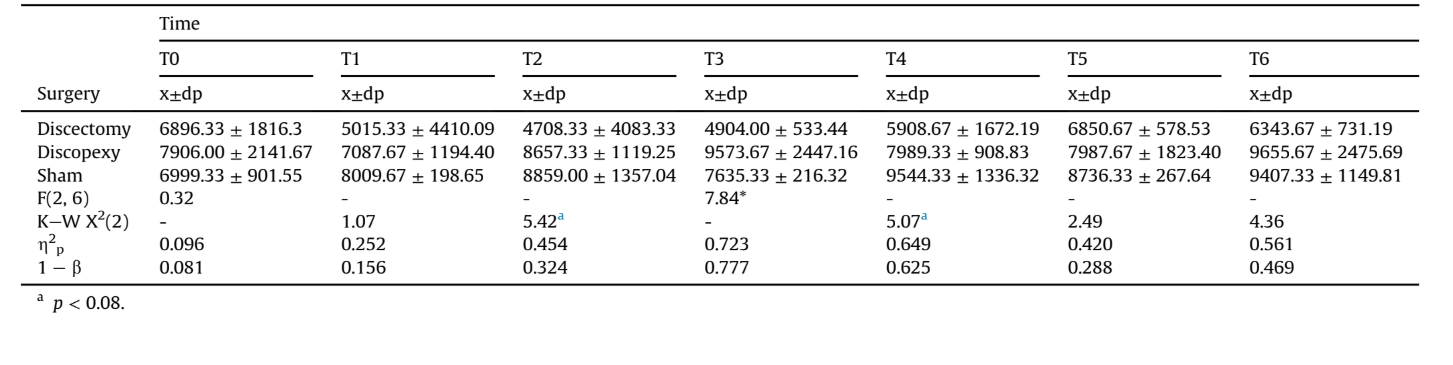
Longitudinal analysis: A one-way ANOVA with repeated measures, with Greenhouse-Geisser correction, taking as within-subject effects the baseline and the 6 months after surgery (T1 to T6) for discectomy, discopexy, and sham surgery, did not show statistically significant differences for the three conditions (p > 0.10). The differences between pre-test and post-test times were also not statistically significant (p > 0.05), with low power, since (1-β) < 0.80, as can be seen in Table 7. Fig. 7 represents rumination area for T0 (pre-test) and T1 to T6 (post-test), for discectomy, discopexy, and sham surgery. The baseline results are similar for the three experimental conditions. After surgery, rumination areas were lower in the discectomy condition, although the differences were not statistically significant.
Adverse events
No serious adverse events were reported, apart from one sheep in the discectomy group that stopped rumination in T1 and T2, but returned to normal function in T3 to T6.
Discussion
The main goal of this study was to analyze the effects of different types of surgery on sheep mastication and rumination. The proposed methodology has proven to be feasible and sensitive to the interventions. Homogenous conditions were obtained in baseline and the animals behaved naturally in front of the camera, guaranteeing the quality of the kinematic assessments (Fig. 3).
The measurement of kinematics was designed to advance understanding of the implications of TMJ surgery on jaw movements. Theoretically, bilateral TMJ surgery may cause jaw movement changes, but these outcomes need to be quantified.
Regarding absolute masticatory time, it was expected that, after bilateral discectomy, the animals would require more time to eat the 150 g of pellets (Ingawale and Goswami, 2009). Accordingly, the discectomy group increased the masticatory time by 28% in T1. This could be related to TMJ pain, leading to a slower food intake. By the end of the study these animals were able to recover to baseline values (74.67 s) (Fig. 4). As mentioned previously, there is a lack of studies evaluating the effects of interventions on functionality of the TMJ. Thus, it was not possible to compare this masticatory outcome measured with other results. Although there were no statistical differences between masticatory time before and after surgery (i.e. T0 vs T1), the difference was noticeable. After T1, the subsequent recover to baseline values suggests that sheep presented the ability to adapt to the induced constraints, highlighting the importance that function has over form (Poveda et al., 2007). Sheep, as with other animals, have the ability to adapt in order to survive, even in the case of TMJ major interventions, where severe dysfunction could lead to disastrous consequences for the animal.
The authors agree that it would be interesting in the future to analyze this outcome for a longer period.
Regarding the rumination time per cycle, notable results were achieved. In the discectomy group one animal stopped rumination through T1 and T2. This suggests a need for future investigations in this field, to understand for example if TMJ could have a more important impact on rumination than on mastication. The authors believed at first that ankylosis might develop after bilateral discectomy, but at T3 all animals were ruminating. This outcome suggests that in spite of an initial slow down related to food intake, rumination area, and even one animal being unable to ruminate, the sheep were able to readapt and return to normal particulate breakdown. When analyzing Fig. 5, it is noticeable that all groups reduced the rumination time per cycle in T3, without knowing the cause of any event leading to that result. However, in T4eT6 the sheep reassumed expected values. The animals from both discectomy and discopexy groups in T5 and T6 needed more time to achieve a ruminatory cycle, suggesting a less effective rumination process.
Regarding rumination area, it is noticeable that a faster ruminant cycle is obtained through a smaller rumination area. Another interesting detail is that in T3 and T4 a normalization of the rumination kinematics was observed for the discectomy group. This outcome suggests that remodelling and adaptation occurs 3-4 months after TMJ surgical intervention. Although ruminant areas were reduced in the discectomy group after surgery, the differences were not statistically significant.
The evaluation of trajectory and area of rumination was interesting because it was possible to identify a pattern. Each animal showed a favorite side for rumination but switched sides independently of the intervention. Every animal displayed a triangular trajectory, similar to the jaw movements demonstrated in anesthetized rabbits (Hidaka et al., 1997).
Further research should be able to examine possible associations between these results and histological, imaging, and weight outcomes (Zhao et al., 2010).
Conclusions
The authors are not aware of any previous randomized, blinded, preclinical studies of the TMJ domain that follow the ARRIVE guidelines. Using black Merino sheep, with age and gender selection, a publicly available protocol, sham control group, and a bilateral approach, we intended to minimising possible bias. The bilateral approach also avoided any adverse effects of the unoperated contralateral joint, as have been reported with unilateral procedures (Dimitroulis and Slavin, 2006). The proposed baseline outcomes were homogeneous and the sham control group performed effectively.
The first month after intervention seems to be the critical period regarding kinematic changes, with modifications related to absolute masticatory time, rumination time per cycle, and rumination area, both in discectomy and discopexy groups. After 1 month, TMJ bilateral discopexy does not seem to have an important kinematic impact in black Merino sheep. TMJ bilateral discectomy does seem to have a significant impact, mostly in T1 and T2, but from T3 to T6 normalization of results is observed.
The authors agree that the rigorous study design, the animal model, and bilateral intervention were the main advantages of this research. The limitations were mostly due to the small sample size, so further research should aim for larger samples. The introduction of kinematic evaluation highlights the importance of kinematics
David Faustino Ângelo, Florencio Monje Gil, Raúl González-García, Lisete Mónico, Rita Sousa, Lia Neto, Inês Caldeira, Carla Moura, Luís Carlos Francisco, David Sanz, Nuno Alves, Francisco Salvado, Pedro Morouço
References
- Ângelo DF, Monje FG, Gonzalez-Garcia R, Little CB, Monico L, Pinho M, et al: Bioengineered temporomandibular joint disk implants: study protocol for a two-phase exploratory randomized preclinical pilot trial in 18 black Merino sheep (TEMPOJIMS). JMIR Res Protoc 6: e37, 2017
- Angelo DF, Morouco P, Alves N, Viana T, Santos F, Gonzalez R, et al: Choosing sheep (Ovis aries) as animal model for temporomandibular joint research: morphological, histological and biomechanical characterization of the joint disc. Morphologie 100: 223-233, 2016
- Bjørnland T, Haanaes HR: Discectomy of the temporomandibular joint: an experimental study in monkeys. J Craniomaxillofac Surg 27: 113-116, 1999
- Bjørnland T, Larheim TA: Discectomy of the temporomandibular joint: 3-year follow-up as a predictor of the 10-year outcome. J Oral Maxillofac Surg 61: 55-60, 2003
- Cohen WA, Servais JM, Polur I, Li Y, Xu L: Articular cartilage degeneration in the contralateral non-surgical temporomandibular joint in mice with a unilateral partial discectomy. J Oral Pathol Med 43: 162-165, 2014
- Dimitroulis G, Slavin J: The effects of unilateral discectomy and condylectomy on the contralateral intact rabbit craniomandibular joint. J Oral Maxillofac Surg 64: 1261-1266, 2006
- Eriksson L, Westesson P-L: Discectomy as an effective treatment for painful temporomandibular joint internal derangement: a 5-year clinical and radiographic follow-up. J Oral Maxillofac Surg 59: 750-758, 2001
- Hidaka O, Morimoto T, Masuda Y, Kato T, Matsuo R, Inoue T, et al: Regulation of masticatory force during cortically induced rhythmic jaw movements in the anesthetized rabbit. J Neurophysiol 77: 3168-3179, 1997
- Ingawale S, Goswami T: Temporomandibular joint: disorders, treatments, and biomechanics. Ann Biomed Eng 37: 976e996, 2009
- Kilkenny C, Parsons N, Kadyszewski E, Festing MFW, Cuthill IC, Fry D, et al: Survey of the quality of experimental design, statistical analysis and reporting of research using animals. PLoS One 4: e7824, 2009
- Mazzonetto R, Spagnoli DB: Long-term evaluation of arthroscopic discectomy of the temporomandibular joint using the holmium yag laser. J Oral Maxillofac Surg 59: 1018-1023, 2001
- Nyberg J, Adell R, Svensson B: Temporomandibular joint discectomy for treatment of unilateral internal derangements e a 5 year follow-up evaluation. Int J Oral Maxillofac Surg 33: 8-12, 2004
- Ogi N, Kurita K, Ishimaru J, Goss AN: Short-term effect of deep-frozen stored auricular cartilage allograft repair on the osteoarthritic sheep temporomandibular joint. Int J Oral Maxillofac Surg 28: 393-397, 1999
- Pearce G: Changes in particle size in the reticulorumen of sheep. Aust J Agric Res 18: 119, 1967
- Poveda RR, Bagan JV, Diaz Fernandez JM, Hernandez Bazan S, Jimenez SY: Review of temporomandibular joint pathology. Part I: classification, epidemiology and risk factors. Med Oral Patol Oral Cir Bucal 12: e292-e298, 2007
- Sato S, Goto S, Koeda S, Motegi K: Changes of the elastic fibre network of the rabbit temporomandibular joint following discectomy. J Oral Rehabil 29: 847-852, 2002
- Sharma R, Sinha R, Menon PS: Meniscopexy for internal derangement of tempo- romandibular joint. J Maxillofac Oral Surg 13: 261-265, 2010
- Takaku S, Sano T, Yoshida M: Long-term magnetic resonance imaging after temporomandibular joint discectomy without replacement. J Oral Maxillofac Surg 58: 739-745, 2000
- Tong AC, Tideman H: A comparative study on meniscectomy and autogenous graft replacement of the rhesus monkey temporomandibular joint articular disc: Part I. Int J Oral Maxillofac Surg 29: 140-145, 2000
- Trumpy IG, Lyberg T: Surgical treatment of internal derangement of the temporomandibular joint: long-term evaluation of three techniques. J Oral Maxillofac Surg 53: 740-747, 1995
- Van der Worp HB, Howells DW, Sena ES, Porritt MJ, Rewell S, O'Collins V, et al: Can animal models of disease reliably inform human studies? PLoS Med 7: e1000245, 2010
- Zhao C, Kurita H, Kurashina K, Hosoya A, Arai Y, Nakamura H: Temporomandibular joint response to mandibular deviation in rabbits detected by 3D micro-CT imaging. Arch Oral Biol 55: 929-937, 2010
