Fabrication of a CAD/CAM combination matrix for trial restorations: A dental technique
Abstract
The trial restoration increases outcome predictability in restorative treatments, enhances communication among specialists and patients, and guides tooth preparations. It should reproduce the planned design precisely because many decisions will be made based on the transferred design. Traditionally, a diagnostic waxing design is transferred to the mouth with a flexible silicone matrix. However, a rigid matrix would ensure an accurate transfer of the planned design by avoiding the deformation of the silicone index. A step-by-step technique for fabricating a computer-aided design and computer-aided manufactured (CAD-CAM) rigid matrix relined with polyvinyl siloxane material to fabricate a trial restoration is presented. The technique ensures accurate detail reproduction and dimensional stability, avoiding deformation and ensuring a predictable transfer of the planned design.
You have the opportunity to gather more in-depth information about digital technologies in dentistry in our course "Indirect restoration in the biomimetic concept".
Esthetic expectations of patients have increased, and contemporary adhesive techniques and glass-ceramic materials provide excellent esthetic outcomes and stability while maximizing the preservation of tooth tissue. Trial restorations have been successfully integrated into restorative dentistry as a tool in the diagnostic phase of treatment. The trial restorations obtained from an anatomic diagnostic waxing enhance communication between the clinician, the patient, other specialists, and the dental laboratory technician. The trial restoration is a valuable tool for guiding minimally invasive dental preparations and fabricating interim restorations.
The traditional techniques transfer the diagnostic waxing to the patient using autopolymerizing or photopolymerizing resin-based materials carried with a silicone matrix or a vacuum-formed resin shell. Accurate placement depends, among many factors, on the applied pressure, the flow of the resin, the amount of tooth support, and the operator’s experience. Proper placement may be challenging in certain clinical situations, and improper placement will cause inaccurate trial restorations that will distort the appearance of the planned restoration, adversely affecting planning decisions. More precise methods using digital tools have been described. Nevertheless, additively manufactured matrices are unsuitable for all situations because of the material thickness required for their fabrication. A novel technique for fabricating a computer-aided design and computer-aided manufactured (CAD-CAM) matrix for trial restorations is described. A 3-dimensionally (3D) printed resin matrix designed from the diagnostic waxing and relined with low-viscosity polyvinyl siloxane (PVS) material is presented. The use of this method ensures detailed reproduction by using the PVS material while also ensuring correct and predictable positioning by using a rigid matrix shell.
Dental technique
Obtain frontal photographs with and without cheek retractors (Fig. 1A, 1B). Scan the maxillary and mandibular arch (Medit i700; Medit Corp) to obtain 2 standard tessellation language (STL) files (Fig. 1C) and the intermaxillary record in maximal intercuspal position or centric relation position as needed.
Import the 2 STL files (STL 1, 2) into a CAD software program (exocad DentalCAD; exocad GmbH) and design a complete mouth virtual diagnostic waxing (Fig. 2). Export the waxed cast as an STL combined file (STL 3).
Import STL 3 into the CAD software program (exocad DentalCAD). Use the occlusal device module to design a 1.5-mm-thick spacer that covers the waxed cast up to the cervical contour. Set the offset distance to 0 mm (Fig. 3A, 3B). Export the diagnostic waxing cast with the spacer as an STL combined file (STL 4) (Fig. 3C).
Import STL 4 into the CAD software program (exocad DentalCAD). Use the occlusal device module to design a 1.5-mm-thick matrix covering the previously combined diagnostic waxing cast and spacer, placing the margins 2 mm above the cervical contour. Set the offset distance to 0.05 mm (Fig. 4A, 4B). Extend the matrix design limits distally to at least 1 unwaxed tooth. Add attachments on the sides of the matrix to facilitate its removal (Fig. 4C-F). Design occlusal or facial apertures on the supportive teeth to visually assess the fit of the matrix on the teeth. Export the trial restoration matrix as an STL file (STL 5) (Fig. 4G).
Three-dimensionally print the waxed STL cast (STL 3) (Sonic Mini 4K; Phrozen Technology) with cast resin (Aqua-Gray 4K printer resin; Phrozen Technology) (Fig. 5A). Then, 3D print the trial restoration matrix (STL 5) with clear biocompatible resin (Dental Clear; Harz Labs) (Fig. 5B). Wash the 3D printed parts with isopropyl alcohol and photopolymerize in an ultraviolet chamber (Wash & Cure machine 2.0; Anycubic 3D Printing). Disinfect the guides by immersion in a 2% chlorhexidine solution for 15 minutes.
Evaluate the fit of the rigid matrix on the diagnostic waxing printed cast, apply PVS adhesive (Universal Adhesive Tray; Zhermack SpA) in the intaglio of the matrix, and reline it with low-viscosity PVS material (Matrix 56; Anaxdent) (Fig. 5C, 5D).
Seat the relined matrix in the patient and assess the fit visually through the occlusal or facial apertures (Fig. 6A). Make the trial restoration with bisacrylic resin (Luxatemp A1; DMG). Because of the tooth-supported fit, the seating of the hybrid matrix should be similar to that obtained for occlusal splints. Remove the matrix with the side attachments after the resin polymerizes. Remove excess and polish (Fig. 6B, 6C).
 Figure 1. Preoperative situation. A, Intraoral frontal view. B, Extraoral frontal view with cheek retractors. C, Digital preview of intraoral diagnostic maxillary scan with toggled standard tessellation language view (STL 1).
Figure 1. Preoperative situation. A, Intraoral frontal view. B, Extraoral frontal view with cheek retractors. C, Digital preview of intraoral diagnostic maxillary scan with toggled standard tessellation language view (STL 1).
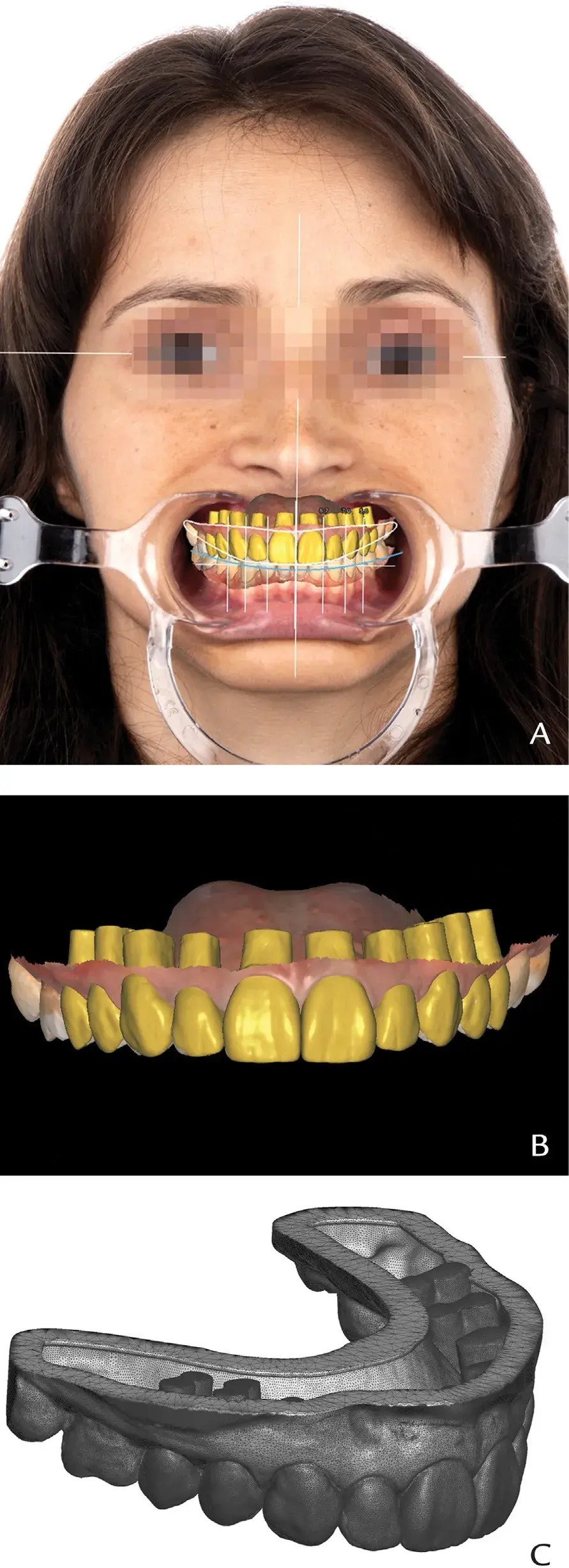 Figure 2. Digital waxing design. CAD alignment of extraoral frontal image and intraoral scan. A, Esthetic parameters and proportions assessment, extraoral frontal image with cheek retractors. B, Waxed design, frontal view. C, Exported single STL waxed cast (STL 3), left side view. CAD, computer-aided design; STL, standard tessellation language.
Figure 2. Digital waxing design. CAD alignment of extraoral frontal image and intraoral scan. A, Esthetic parameters and proportions assessment, extraoral frontal image with cheek retractors. B, Waxed design, frontal view. C, Exported single STL waxed cast (STL 3), left side view. CAD, computer-aided design; STL, standard tessellation language.
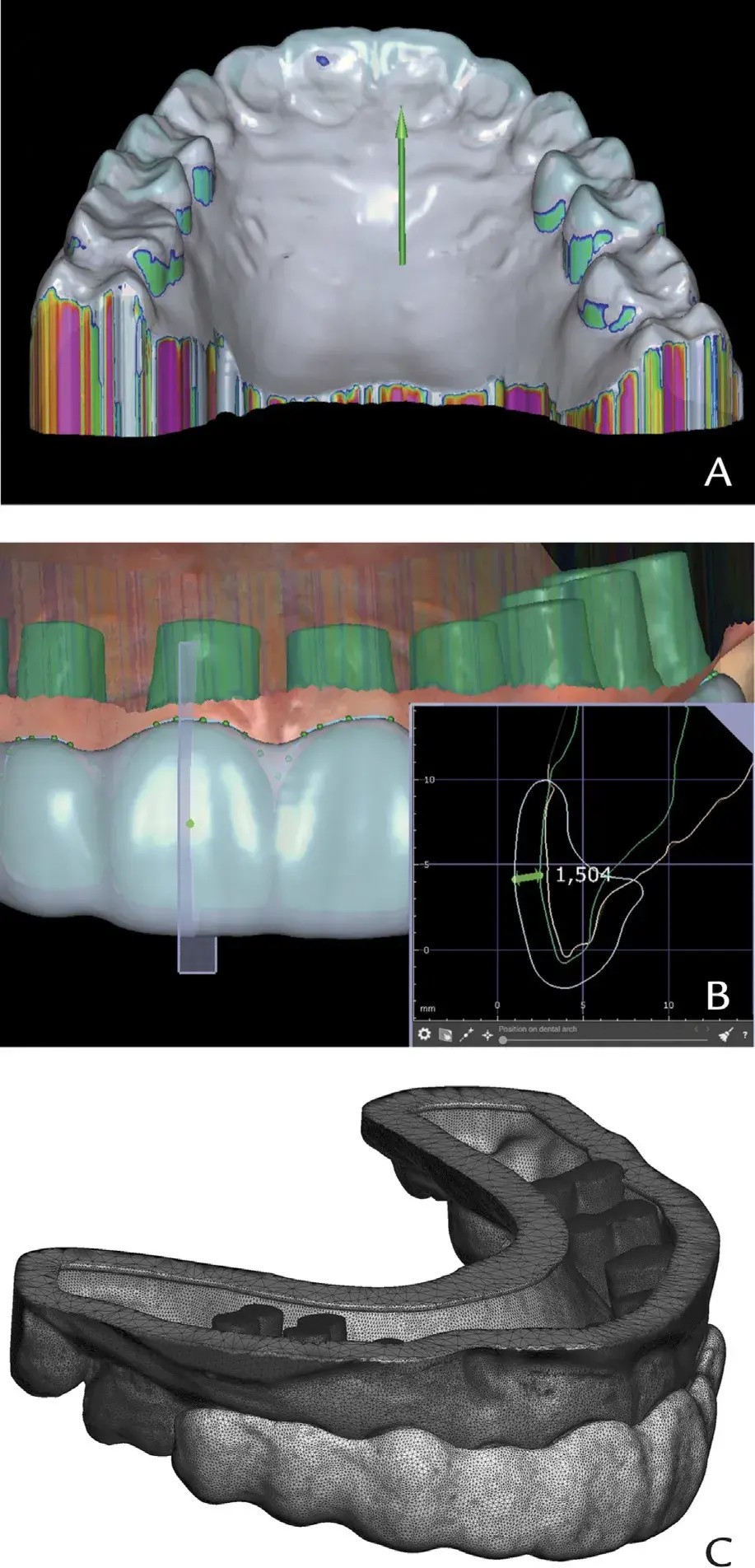 Figure 3. Spacer design. A, Insertion path for spacer design inside occlusal device module of dental CAD software program. Undercut compensations set toward palatal side, occlusal view. B, Spacer thickness assessment, cut view. C, Exported combined single STL of waxed cast (STL 4), left side view. CAD, computer-aided design; STL, standard tessellation language.
Figure 3. Spacer design. A, Insertion path for spacer design inside occlusal device module of dental CAD software program. Undercut compensations set toward palatal side, occlusal view. B, Spacer thickness assessment, cut view. C, Exported combined single STL of waxed cast (STL 4), left side view. CAD, computer-aided design; STL, standard tessellation language.
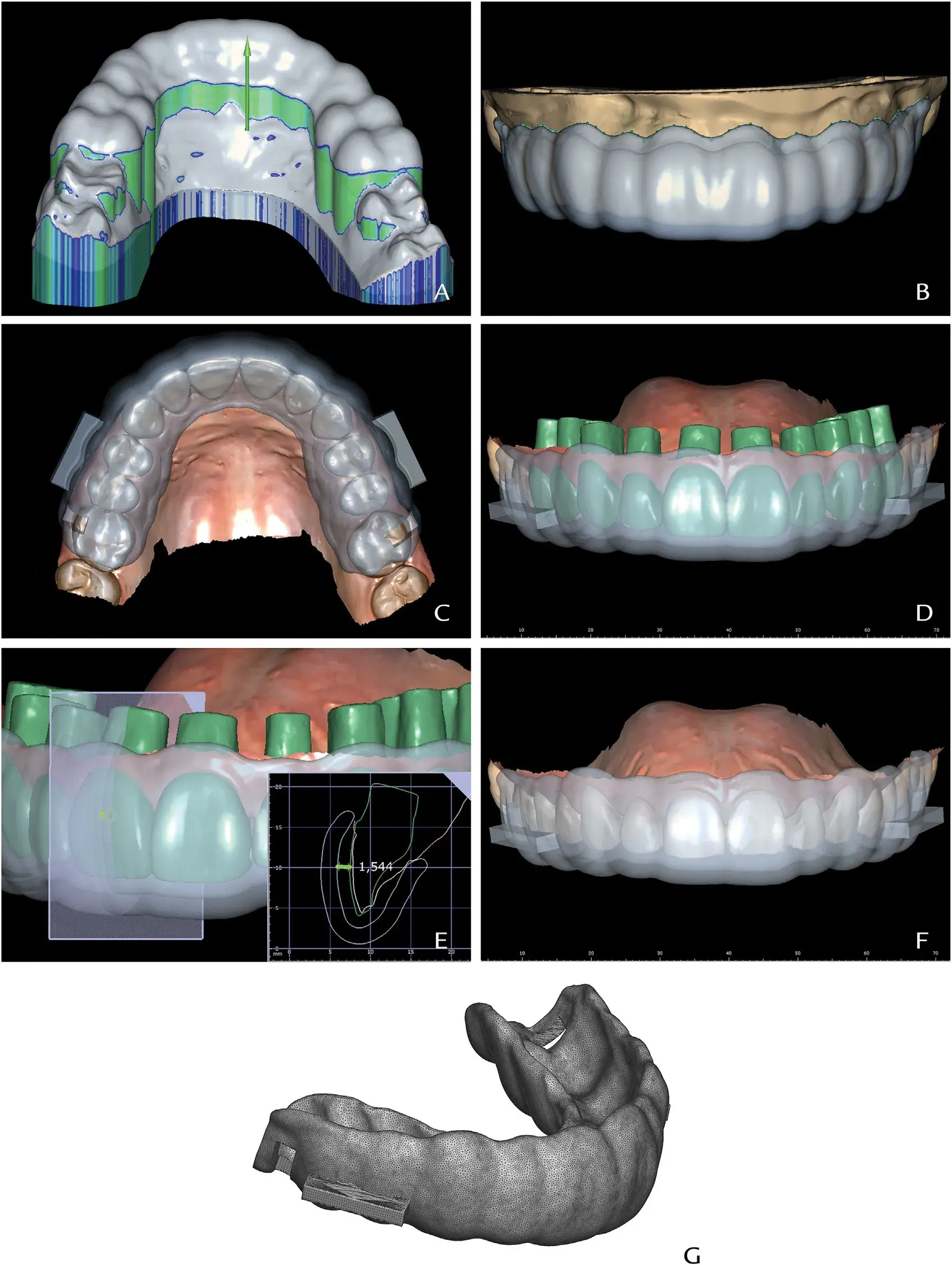 Figure 4. Trial restoration matrix design. A, Insertion path for trial restoration matrix design inside occlusal device module of dental CAD software program. Undercut compensations set toward palatal side, occlusal view. B, Matrix margins placed at 2 mm from height of cervical spacer contour. C, Trial restoration matrix definitive design with lateral attachments for matrix removal and occlusal or facial apertures for fit assessment; occlusal view. D, Trial restoration matrix definitive design, frontal view. E, Final space assessment from intaglio of trial restoration matrix and buccal aspect of waxed cast, cut view. F, Trial restoration matrix definitive design, frontal view. G, Exported trial restoration matrix STL file (STL 5), left side view. CAD, computer-aided design; STL, standard tessellation language.
Figure 4. Trial restoration matrix design. A, Insertion path for trial restoration matrix design inside occlusal device module of dental CAD software program. Undercut compensations set toward palatal side, occlusal view. B, Matrix margins placed at 2 mm from height of cervical spacer contour. C, Trial restoration matrix definitive design with lateral attachments for matrix removal and occlusal or facial apertures for fit assessment; occlusal view. D, Trial restoration matrix definitive design, frontal view. E, Final space assessment from intaglio of trial restoration matrix and buccal aspect of waxed cast, cut view. F, Trial restoration matrix definitive design, frontal view. G, Exported trial restoration matrix STL file (STL 5), left side view. CAD, computer-aided design; STL, standard tessellation language.
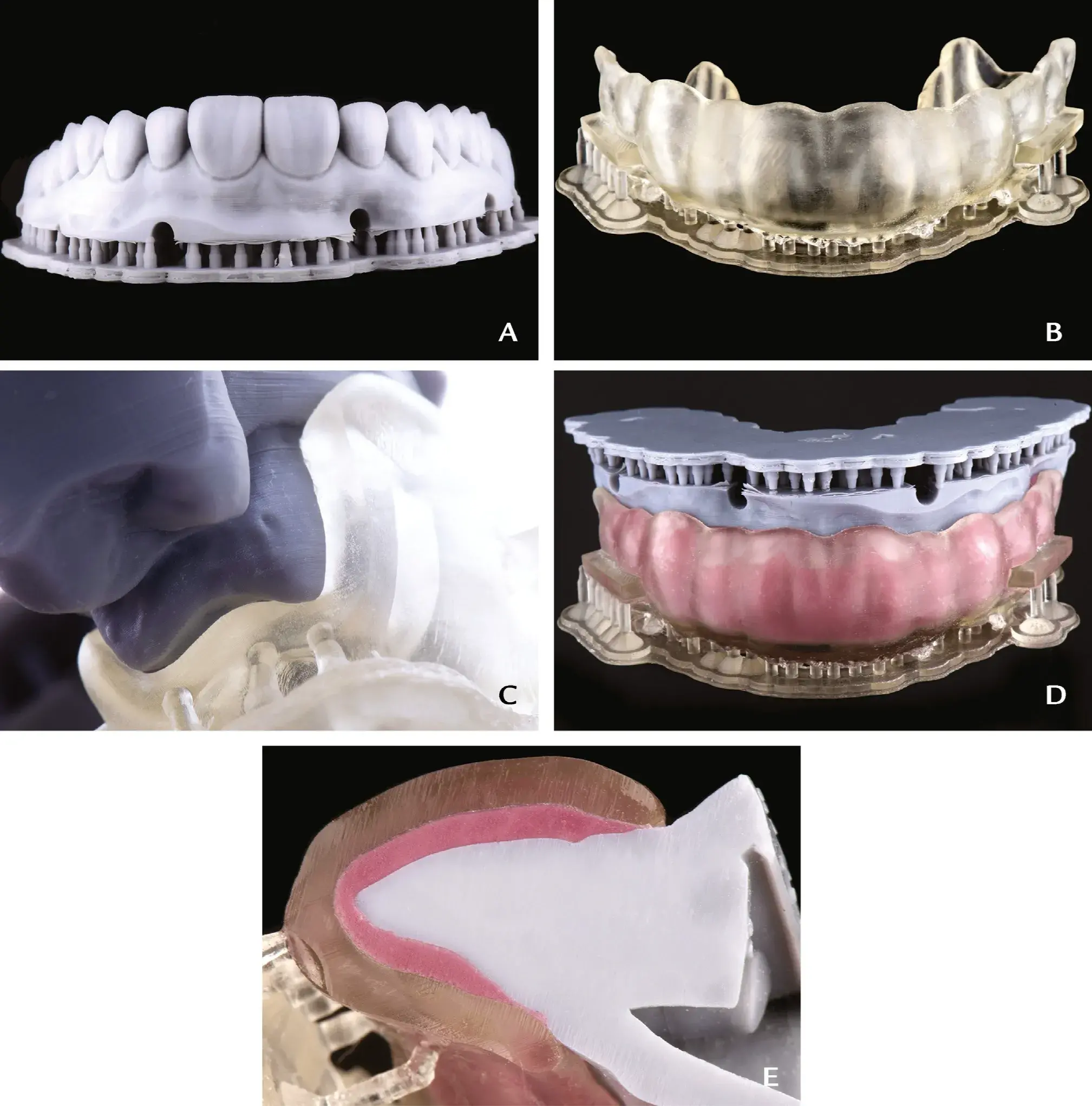 Figure 5. Trial restoration matrix fabrication. A, 3D-printed waxed cast, frontal view. B, 3D-printed trial restoration matrix, frontal view. C, Distal fitting assessment between 3D-printed waxed cast and trial restoration matrix. D, Trial restoration matrix relined with light-body PVS impression material. E, Sagittal cut of trial restoration matrix, light-body PVS, waxed cast for thickness assessment, cut view. 3D, three-dimensional; PVS, polyvinyl siloxane.
Figure 5. Trial restoration matrix fabrication. A, 3D-printed waxed cast, frontal view. B, 3D-printed trial restoration matrix, frontal view. C, Distal fitting assessment between 3D-printed waxed cast and trial restoration matrix. D, Trial restoration matrix relined with light-body PVS impression material. E, Sagittal cut of trial restoration matrix, light-body PVS, waxed cast for thickness assessment, cut view. 3D, three-dimensional; PVS, polyvinyl siloxane.
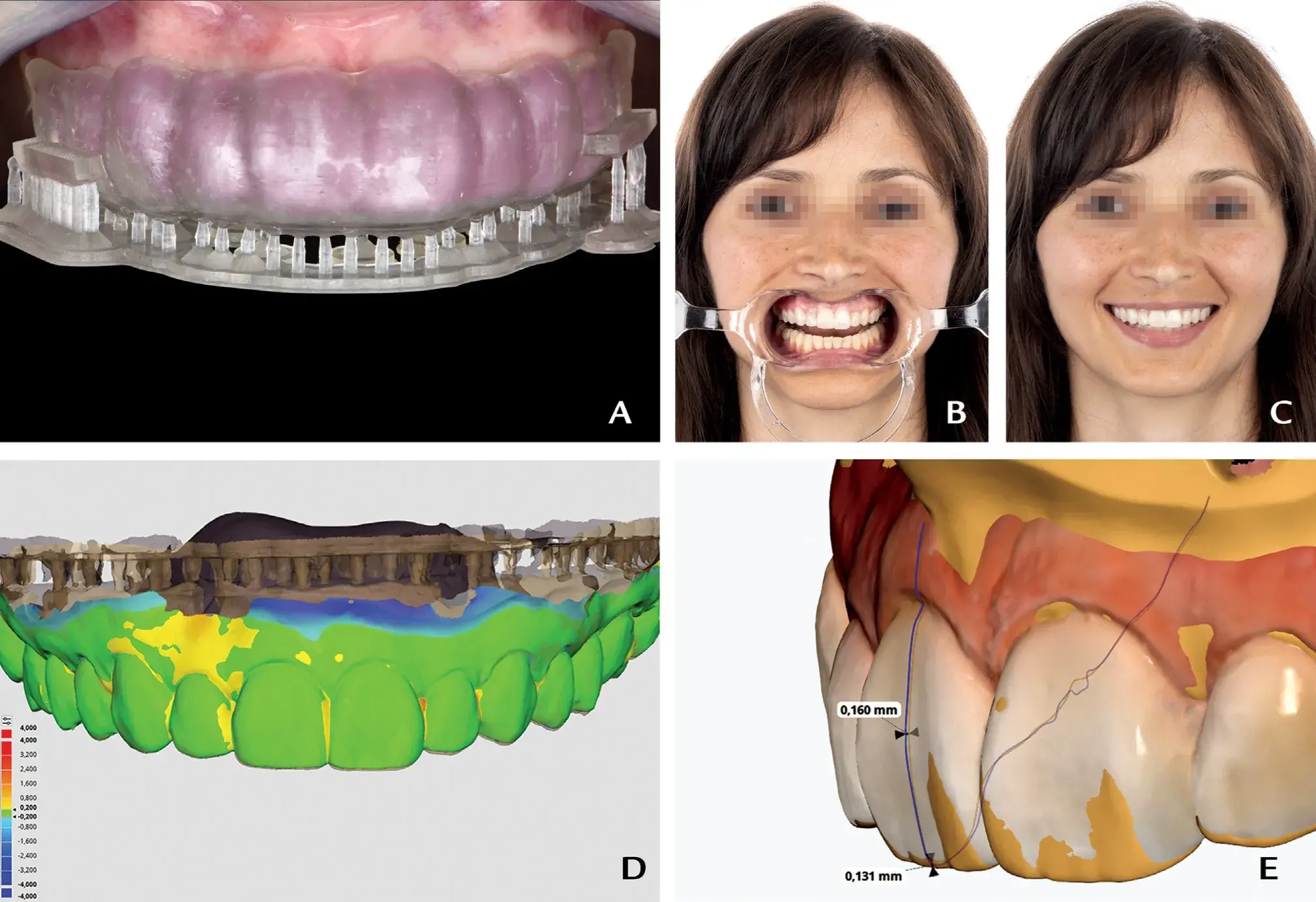 Figure 6. Definitive trial restoration. A, Intraoral frontal view of trial restoration matrix placed. B, Extraoral frontal view of trial restoration with cheek retractors. C, Extraoral frontal view of trial restoration. D, STL mesh comparison of intraoral scan of trial restoration and waxed cast scanned with IOS (color map, tolerance 200 mm). E, Buccal and incisal linear measurements on sagittal cut of aligned STL meshes of trial restoration intraoral scan and waxed cast scanned with IOS. IOS, intraoral scanner; STL, standard tessellation language.
Figure 6. Definitive trial restoration. A, Intraoral frontal view of trial restoration matrix placed. B, Extraoral frontal view of trial restoration with cheek retractors. C, Extraoral frontal view of trial restoration. D, STL mesh comparison of intraoral scan of trial restoration and waxed cast scanned with IOS (color map, tolerance 200 mm). E, Buccal and incisal linear measurements on sagittal cut of aligned STL meshes of trial restoration intraoral scan and waxed cast scanned with IOS. IOS, intraoral scanner; STL, standard tessellation language.
Discussion
A dental technique for designing a CAD-CAM combination matrix for trial restorations is described. First, a 3D-printed matrix that provides uniform and calibrated space for the relining material is designed. Subsequently, the resin matrix is relined on the diagnostic waxing cast with low-viscosity PVS, which maximizes detail reproduction. The matrix is rigid to avoid deformations.
Different trial restoration techniques have been described. Conventional techniques use autopolymerizing resin carried with a silicone index made from the diagnostically waxed cast. However, precise placement of the matrix is challenging, and whether an esthetic deficiency results from poor diagnostic waxing design or misplacement of the trial restorations may be unclear.
With the presented technique, correct positioning of the 3D-printed resin matrix housing the PVS is facilitated (Fig. 6D, 6E). The trial restoration is helpful for esthetic evaluation and minimally invasive dental preparation with preparation guides. Moreover, the 3D-printed matrix facilitates the fabrication of interim restorations that replicate the definitive restorations, ensuring sufficient tooth preparation and optimal esthetics. Limitations of the described technique include the need for a proprietary CAD software program and a 3D printer. However, the proprietary CAD design software program is widespread in dental laboratories and dental practices, and 3D printers are affordable and can be used for other applications such as fabrication surgical guides, casts, and interim restorations.
There are additional information about CAD/CAM technology you can find in our course.
Summary
Proprietary dental CAD software programs can be used to design a CAD-CAM trial restoration matrix by following the described step-by-step protocol. The matrix design can be 3D printed with biocompatible resin and relined with low-viscosity PVS silicone.
References
Dawood A, Purkayastha S, Patel S, MacKillop F, Tanner S. Microtechnologies in implant and restorative dentistry: a stroll through a digital dental landscape. Proc Inst Mech Eng H. 2010;224:789e796.
Ting-Shu S, Jian S. Intraoral digital impression technique: a review. J Prosthodont. 2015;24:313e321.
Gürel G. Porcelain laminate veneers: minimal tooth preparation by design. Dent Clin North Am. 2007;5:419e431.
Lanza MDS, Vasconcellos WA, Miranda GLP, Peixoto RTRC, Lanza LD. Different bonding agents effect on adhesive bond strength: lithium disilicate glass ceramic. Rev Odontol UNESP. 2020;49:e20200020.
Marzola R, Derbabian K, Donovan TE, Arcidiacono A. The science of communicating the art of esthetic dentistry. Part I: patient-dentist-patient communication. J Esthet Dent. 2000;12:131e138.
Simon H, Magne P. Clinically based diagnostic wax-up for optimal esthetics: the diagnostic mock-up. J Calif Dent Assoc. 2008;36:355e362.
Kois DE, Schmidt KK, Raigrodski AJ. Esthetic templates for complex restorative cases: rationale and management. J Esthet Restor Dent. 2008;20:239e248.
Thomas MS, David K. Importance of anatomic mock-up for predictable esthetic smile design with ceramic veneers. J Interdiscip Dent. 2014;4:55.
Farias-Neto A, de Medeiros FCD, Vilanova L, Simonetti Chaves M, Freire Batista de Araújo JJ. Tooth preparation for ceramic veneers: when less is more. Int J Esthet Dent. 2019;14:156e164.
Gurel G, Sesma N, Calamita MA, Coachman C, Morimoto S. Influence of enamel preservation on failure rates of porcelain laminate veneers. Int J Periodontics Restorative Dent. 2013;33:31e39.
Heinsohn JP, Arteaga EM, Rivera GJ, Stange VB. Mock-up an old tool renewed. J Clin Res Dent. 2018;1:1e5.
Small BW. Provisional restorations for veneers. Gen Dent. 2008;56:608e610.
Reyes A, Turkyilmaz I, Prihoda TJ. Accuracy of surgical guides made from conventional and a combination of digital scanning and rapid prototyping techniques. J Prosthet Dent. 2015;113:295e303.
Revilla-León M, Özcan M. Additive manufacturing technologies used for processing polymers: current status and potential application in prosthetic dentistry. J Prosthodont. 2019;28:146e158.
Esquivel J, Villarroel M, Tran D, Kee E, Bruggers K. The utilization of snap-on provisionals for dental veneers: from an analog to a digital approach. J Esthet Restor Dent. 2020;32:161e170.
Alanazi LM, Alkhashrami AA, Rayan Abdullah Albader D, et al. Snap on smile: a systematic review. Saudi J Oral Dent Res. 2020;5:522e527.
Naumovski B, Kapushevska B. Dimensional stability and accuracy of silicone - based impression materials using different impression techniques - a literature review. Pril (Makedon Akad Nauk Umet Odd Med Nauki). 2017;38:131e138.
Gonçalves FS, Popoff DA, Castro CD, Silva GC, Magalhães CS, Moreira AN. Dimensional stability of elastomeric impression materials: a critical review of the literature. Eur J Prosthodont Restor Dent. 2011;19:163e166.
Donovan TE, Chee WW. A review of contemporary impression materials and techniques. Dent Clin North Am. 2004;48:445e470.
Pagac M, Hajnys J, Ma QP, et al. A review of vat photopolymerization technology: materials, applications, challenges, and future trends of 3D printing. Polymers. 2021;13:598.
Pant R, Juszczyk AS, Clark RK, Radford DR. Long-term dimensional stability and reproduction of surface detail of four polyvinyl siloxane duplicating materials. J Dent. 2008;36:456e461.
Caponi L, Raslan F, Roig M. Fabrication of a facially generated tooth reduction guide for minimally invasive preparations: a dental technique. J Prosthet Dent. 2022;127:689e694.
Lucas Queiroz Caponi, DDS, MSc
Eduardo de Lima Flor, DDS, MSc
Carla Vidal-Ponsoda, DDS, MSc
Oscar Figueras-Alvarez, DDS, PhD
Miguel Roig, MD, DMD, PhDe


