Periodontal considerations
ABSTRACT
This chapter focuses instead on a review of those portions of periodontal diagnosis and therapy that pertain to comprehensive fixed prosthodontic treatment. The periodontium that supports fixed prosthodontics is a conduit to immediate and long-term success.
When proper periodontal treatment is provided, most adults will not lose teeth because of periodontal disease. However, although periodontally compromised teeth can be retained over long periods of time, such teeth may not provide a solid foundation to support a fixed dental prosthesis
PREVALENCE
Periodontal textbooks comprehensively describe periodontal disease causes, diagnosis, treatment planning, and treatment options and explain in detail the many interactions between oral and systemic health. This chapter focuses instead on a review of those portions of periodontal diagnosis and therapy that pertain to comprehensive fixed prosthodontic treatment.
Periodontal therapy is extremely effective. Today, few individuals lose their teeth as a result of untreatable periodontal disease (Fig. 5.1). This statistic may appear to contradict the often-repeated axiom that most tooth loss is caused by periodontal disease. However, individuals with access to proper dental care can retain even compromised teeth for extended periods of time. According to data from the 2009 and 2010 National Health and Nutrition Examination Survey (NHANES), only 38.5% of adults in the United States have one or more teeth affected by moderate to severe periodontal disease. The criterion for the diagnosis of moderate to severe periodontal disease was one site with attachment loss of 3mm or more and pocket depth of 4mm or more.
Long-term periodontal maintenance studies have shown that of patients with moderate to severe disease referred for periodontal treatment, more than half did not lose a single tooth in two decades of periodontal maintenance, and 75% lost fewer than three teeth.3 This suggests that when proper periodontal treatment is provided, most adults (90% to 95%) will not lose teeth because of periodontal disease. However, although periodontally compromised teeth can be retained over long periods of time, such teeth may not provide a solid foundation to support a fixed dental prosthesis. More long-term results of perio-restorative cases treatment in author's course "Perio-restorative protocols: team-based approach" by Dr. Daniel Melker.
When periodontally compromised teeth are lost, such often results from lack of access to effective care. A strong correlation exists between poverty, lack of education, and the presence of periodontal disease. The prevalence of periodontal disease among poor patients is 6% higher than in the overall population. Cost of care is a major obstacle in the prevention of tooth loss. Too often, periodontal disease is left untreated because of the patient’s inability to afford proper care.
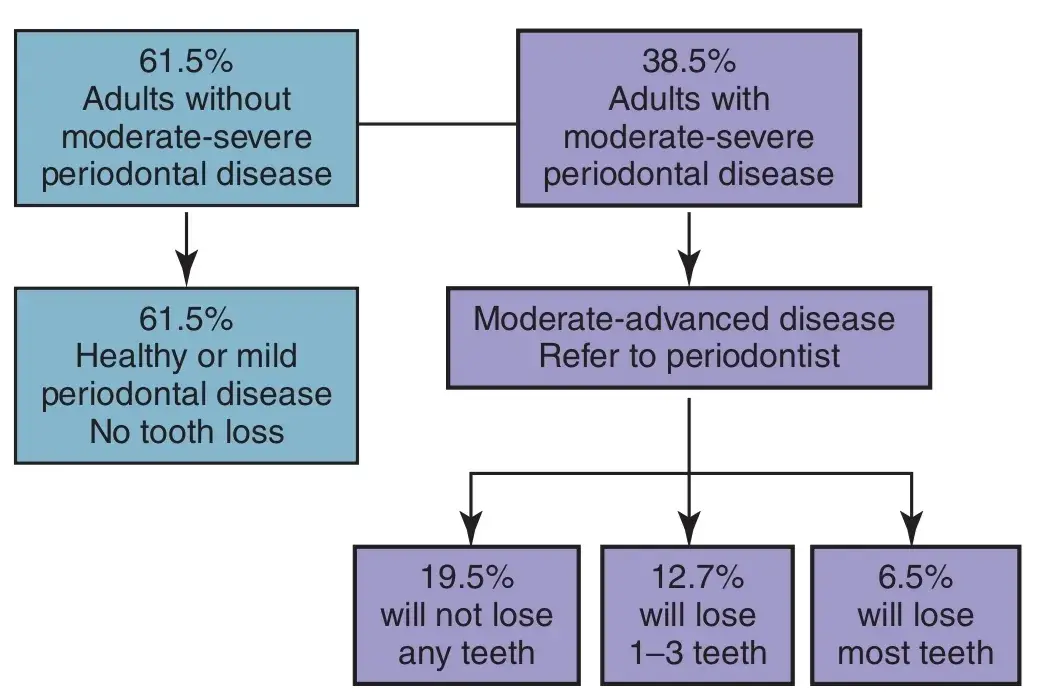 Fig. 5.1 Combined data from the 2010 National Health and Nutrition Examination Survey (NHANES) and from Hirschfeld and Wasserman’s3 report on 22 years of periodontal maintenance. Approximately 2.5% of the U.S. population (6.5% of the 38.5%) have a severe form of periodontal disease that responds poorly to current therapy.
Fig. 5.1 Combined data from the 2010 National Health and Nutrition Examination Survey (NHANES) and from Hirschfeld and Wasserman’s3 report on 22 years of periodontal maintenance. Approximately 2.5% of the U.S. population (6.5% of the 38.5%) have a severe form of periodontal disease that responds poorly to current therapy.
TREATMENT OF PERIODONTITIS
Periodontal disease progresses from gingivitis to periodontitis when connective tissue attachment is lost. Periodontal disease may be characterized by alternating periods of quiescence and exacerbation. The extent to which a periodontal lesion progresses before it is treated determines the amount of bone and connective tissue attachment loss that occurs. This subsequently affects the prognosis of the tooth with regard to restorative demands.
Effective periodontal care incorporates three components: (1) effective daily plaque removal by the patient, (2) active therapy to remove calculus, endotoxins, and pathologic bacteria from the root surfaces and pocket, and (3) preventive periodontal maintenance therapy (supportive periodontal therapy [SPT]) every 2 to 6 months.11 Few patients are consistently successful in removing all plaque accumulation. However, a healthy immune system has been shown to be able to compensate for the presence of some residual plaque. Periodontal disease is site specific; the distal surface of a tooth may exhibit disease while its mesial surface is healthy (Fig. 5.2). The logical implication is that diagnosis and treatment must also be site specific. Enhanced salivary diagnostic testing has the ability to indicate active bone loss and to detect pathologic bacteria.
However, most of these tests are more general, indicating whole mouth values, and high costs preclude their routine use. The most cost-effective, reliable, site-specific indicators of periodontal health are comparison of pocket depths, attachment levels, bleeding on probing (BOP), and tooth mobility over time (Fig. 5.3).
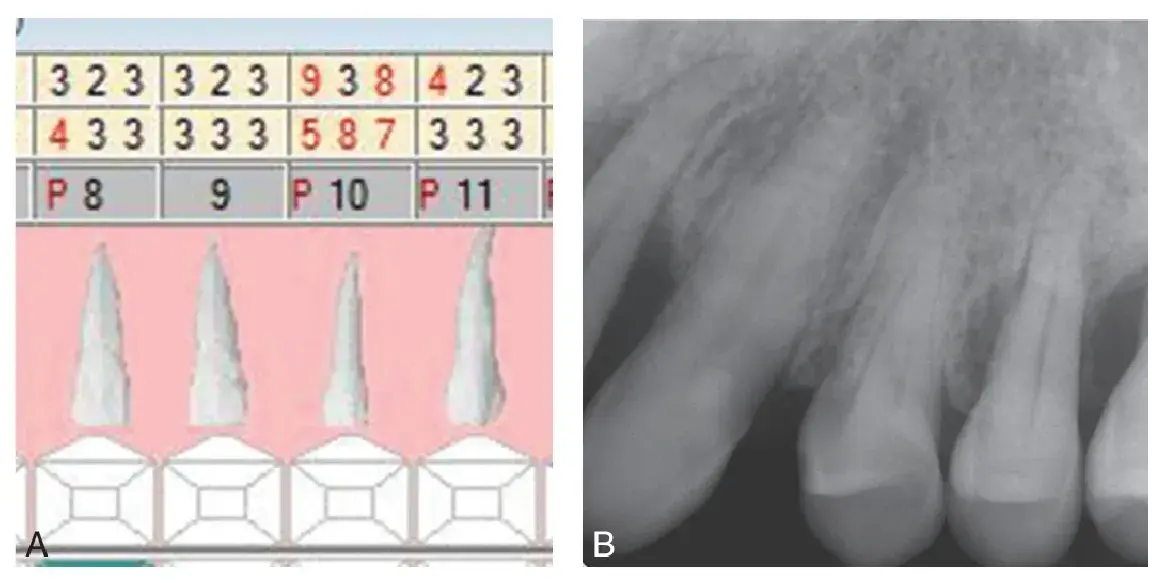 Fig. 5.2 Site-specific nature of periodontal disease. (A) Pocket depths of teeth #8 to #11. (B) Severe bone loss is visible on tooth #10, and yet the mesial surface of tooth #11 exhibits only minor changes.
Fig. 5.2 Site-specific nature of periodontal disease. (A) Pocket depths of teeth #8 to #11. (B) Severe bone loss is visible on tooth #10, and yet the mesial surface of tooth #11 exhibits only minor changes.
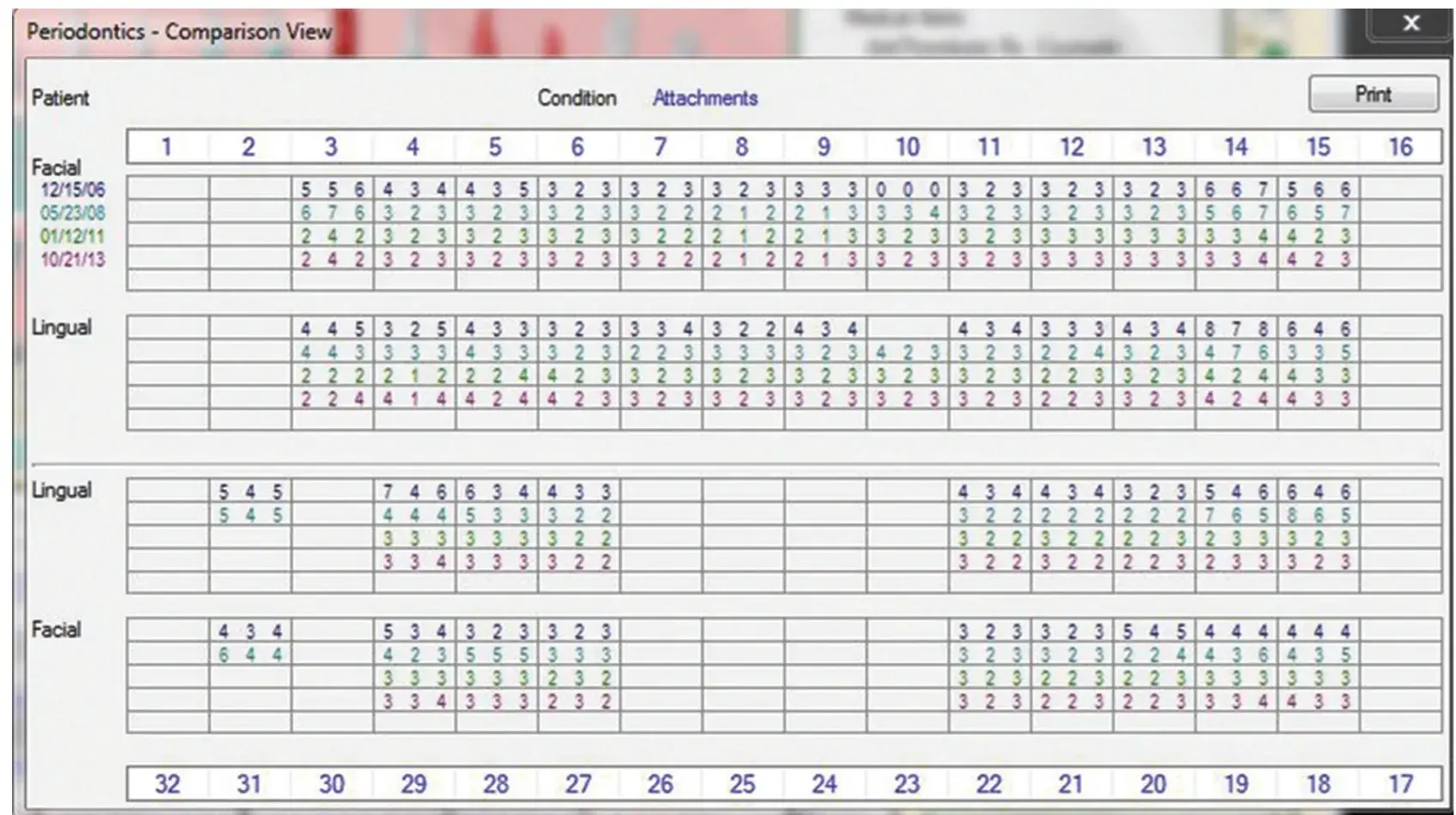 Fig. 5.3 Comparison of stable attachment levels over a 7-year period of supportive periodontal therapy.
Fig. 5.3 Comparison of stable attachment levels over a 7-year period of supportive periodontal therapy.
Scaling and root-planing (SC/RP) remains the foundation of periodontal treatment. During active therapy, it results in the greatest gain in attachment level of all possible therapeutic techniques, reasonable pocket depth reduction, decreased BOP, and an improvement in microbial composition. It has been shown to be cost effective, and negative side effects are minimal in comparison with those of all other techniques. The objective is to achieve a clean root surface, which can be accomplished with hand instrumentation, an ultrasonic scaler, or a laser. What is important is the quality of the root debridement, not the tool used to achieve the clean surface. Antibiotics are often useful in eliminating pathogenic bacteria not accessible with mechanical therapy. SC/RP is definitive therapy for most patients. Any therapy that brings about resolution of inflammation—such as improved oral hygiene, antibiotic therapy, SC/RP, laser therapy, or surgery—will result in gingival recession if bone has been lost. The extent of recession is extremely important to the restorative dentist when precise margin location and gingival symmetry are necessary to achieve a desired esthetic result (Fig. 5.4).
The most frequent indications for surgical periodontal therapy are (1) continued bone loss in a patient who has had SC/RP and is on a 2- to 3-month periodontal maintenance schedule and (2) the need for fixed prosthodontic treatment that will result in either a subgingival crown margin inaccessible for cleaning, or a short clinical crown that will have inadequate retention or resistance form. Surgical procedures are designed to allow meticulous cleaning of the root surfaces and to reduce pockets through removal of gingiva or regrowth of bone. However, unless followed by frequent SPT, plaque will accumulate in the surgical sites, periodontal disease will recur, and significant attachment will be further lost.24 Short-term positive changes from various surgical therapies ameliorate over time. After 7 years, results of all therapies, including SC/RP, are similar when considering pocket reduction, attachment levels, and tooth retention. Frequent SPT underlies successful periodontal therapy. Without frequent SPT, almost all periodontal therapy will fail.
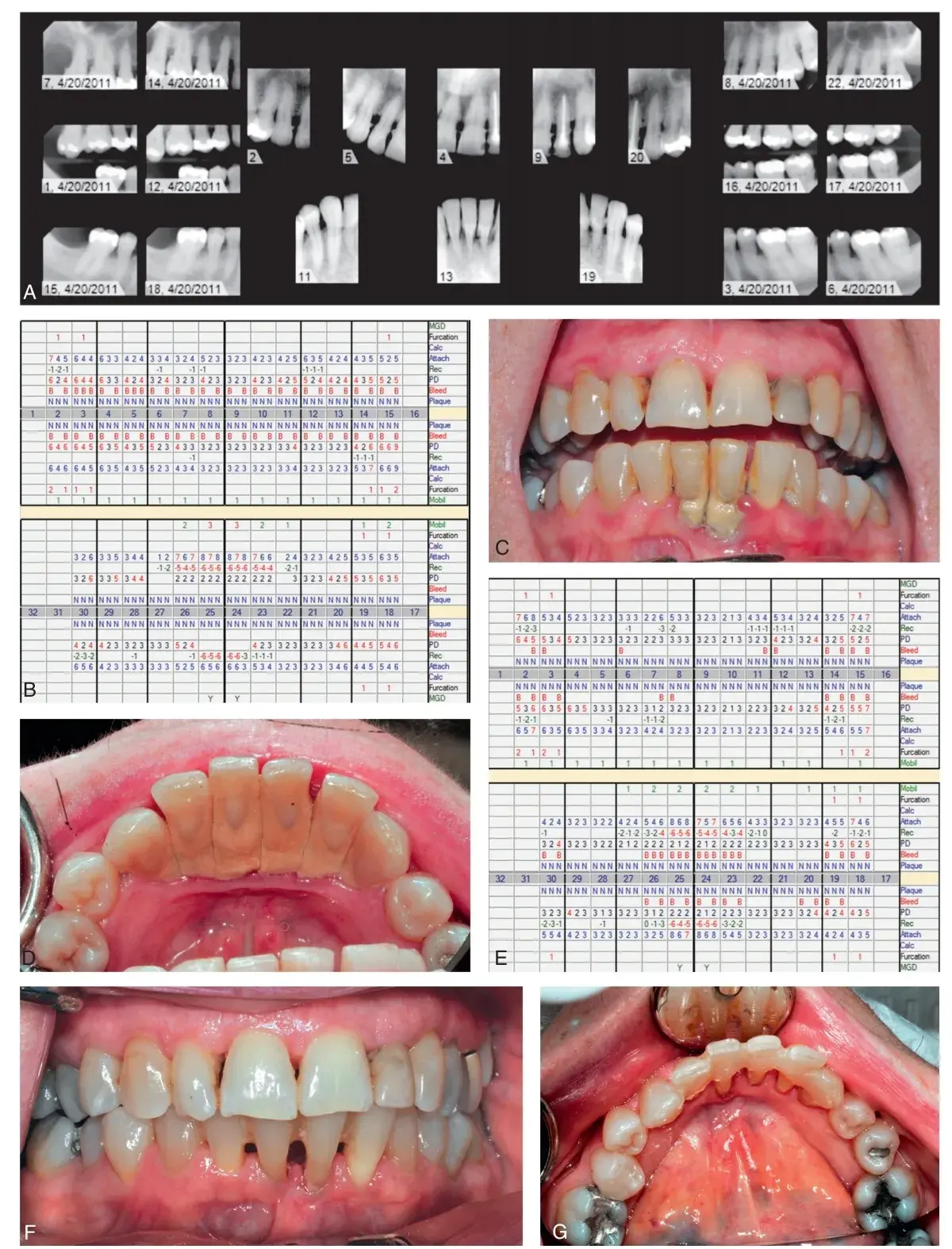 Fig. 5.4 Periodontal charting showing resolution of periodontal infection with scaling and root planing (SC/RP) results in a reduction in inflammation and gingival recession. (A and B) Pre-SC/RP radiographs and data showing generalized moderate-to-severe periodontitis. (C and D) Initial presentation. (E) Post-SC/RP reevaluation data, demonstrating pocket reduction and gingival recession. (F and G) Post-SC/RP appearance, with clinical reduction in inflammation and gingival recession. (C, D, F, and G, Courtesy Dr. Spencer Shoff.)
Fig. 5.4 Periodontal charting showing resolution of periodontal infection with scaling and root planing (SC/RP) results in a reduction in inflammation and gingival recession. (A and B) Pre-SC/RP radiographs and data showing generalized moderate-to-severe periodontitis. (C and D) Initial presentation. (E) Post-SC/RP reevaluation data, demonstrating pocket reduction and gingival recession. (F and G) Post-SC/RP appearance, with clinical reduction in inflammation and gingival recession. (C, D, F, and G, Courtesy Dr. Spencer Shoff.)
The time interval or frequent SPT varies according to the individual patient. In most successful long-term studies, 2 to 3 months has been the standard time interval between SPT appointments. The appointment interval is then lengthened or shortened according to the results for the individual patient. Treatment at each SPT appointment should be based on comparisons of pocket depths, attachment levels, the presence of BOP, and mobility at the current appointment with those of the previous appointment (Fig. 5.5).
An increase of pocket depths or loss of attachment of 2mm is a reliable indicator that continued periodontal destruction is occurring.19 The absence of BOP is a reliable indicator of health.28 Continued BOP at the same site is the best predicator of future attachment loss (Fig. 5.6). Increasing mobility indicates the need for careful analysis of the occlusion and/or endodontic status of the tooth if pocket depths and attachment levels have not changed. Obtaining complete periodontal data at every SPT appointment changes the appointment from a nonspecific teeth cleaning to a site-specific program to maintain periodontal health.
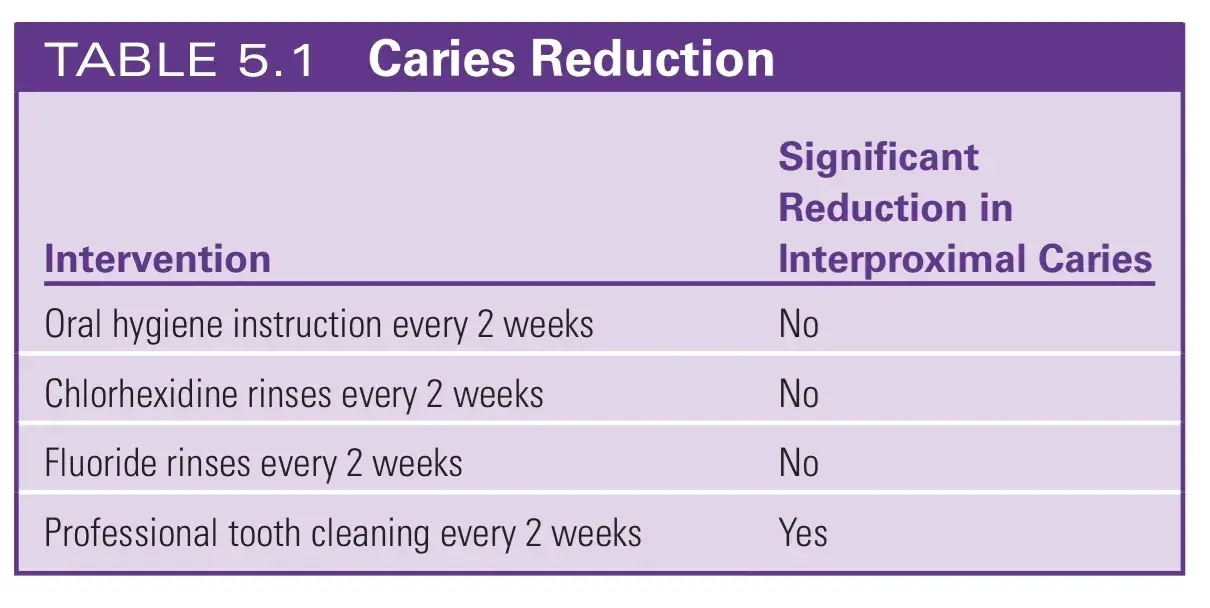
An overlooked benefit of SPT is the concurrent reduction in dental caries that occurs with frequent periodontal maintenance. Several researchers evaluated interproximal caries in teenagers.
They found that oral hygiene instruction, chlorhexidine rinses, and fluoride rinses performed every 2 weeks had almost no effect on new carious lesions. A professional cleaning every 2 weeks reduced new carious lesions significantly (Table 5.1). In another study, children (aged 3 to 13) of adult patients being treated for periodontal disease were evaluated. These children received cleanings every 6 months for 20 years. No periodontal destruction was seen, and the average rate of caries was one lesion per child over the 20-year interval.
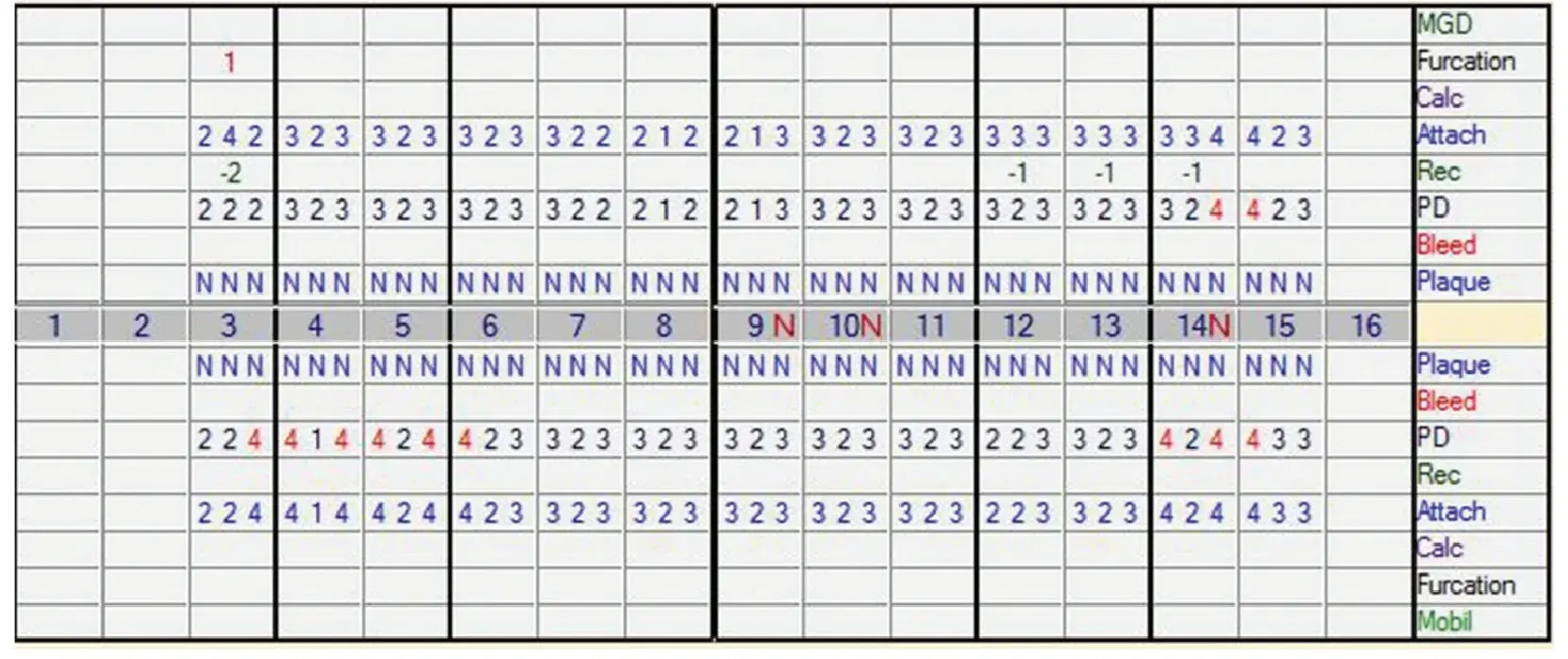 Fig. 5.5 Comparison of bleeding upon probing at individual sites over time.
Fig. 5.5 Comparison of bleeding upon probing at individual sites over time.
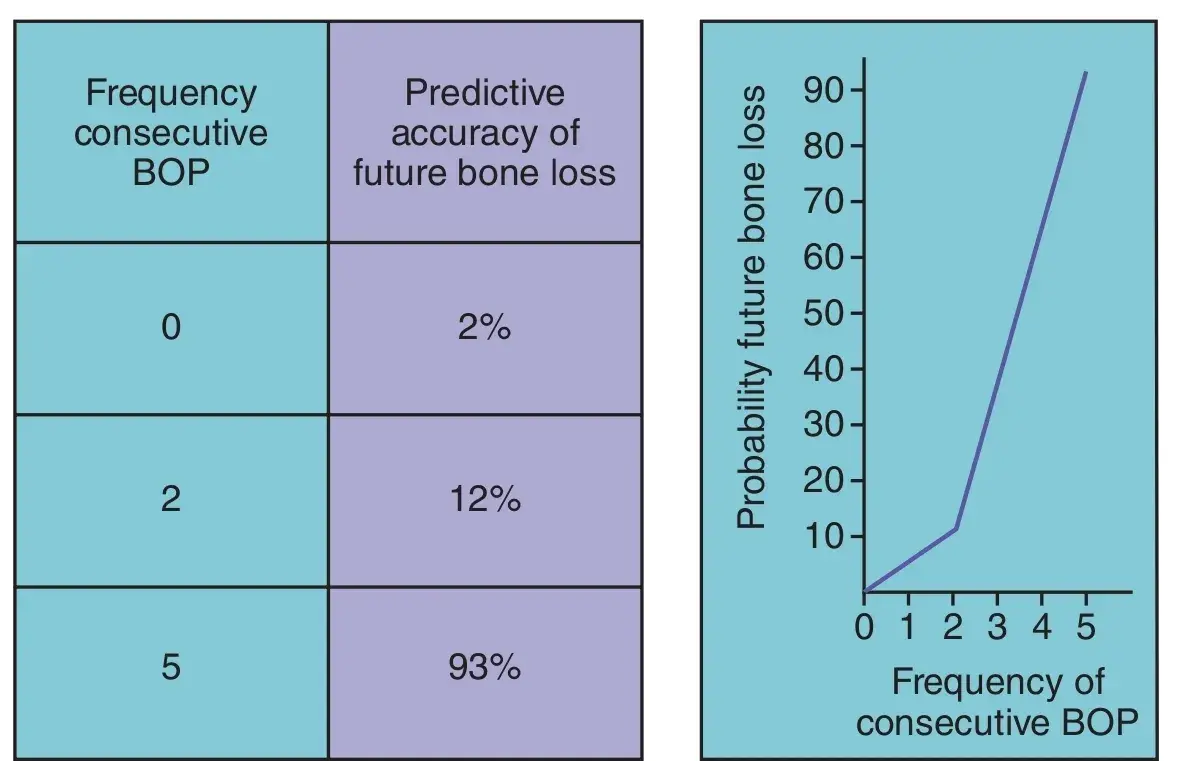 Fig. 5.6 The absence of bleeding on probing (BOP) is a reliable indicator of periodontal health. Continued BOP at the same site greatly increases the risk of future bone loss.
Fig. 5.6 The absence of bleeding on probing (BOP) is a reliable indicator of periodontal health. Continued BOP at the same site greatly increases the risk of future bone loss.
Axelsson et al evaluated the effects of SPT every 2 to 3 months in adults. Fifteen years earlier, they had treated 375 adults with SC/RP and caries control. All patients were recalled every 2 to 3 months for 6 years. Of these patients, 95% were stable, with no additional caries or periodontal destruction. For those patients, the recall interval was lengthened to one to two times per year. The 5% of patients who exhibited additional periodontal destruction or new carious lesions continued their recall interval of every 2 to 3 months. After 15 years, all patients who had completed the prescribed recall intervals had maintained a low caries rate and exhibited almost no additional periodontal destruction.33 A reasonable approach to prevent future caries and periodontal disease is a 2- to 3-month SPT interval for all patients who exhibit active caries or periodontal disease. If the patient experiences no additional caries or periodontal breakdown after 2 years, the SPT interval can be lengthened to 4 to 6 months. The key component of SPT is the meticulous record keeping in which caries, pocket depths, attachment levels, BOP, and mobility at the current appointment was compared with those at the previous appointment; changes are made as necessary.
PROGNOSIS
When prosthetic replacement of missing teeth is necessary, an accurate prognosis of the remaining teeth is essential. The prognosis is the best guess of the course or outcome of the periodontal disease. It comprises (1) the prognosis for the overall dentition and (2) the prognosis for individual teeth. A tentative prognosis is made after a thorough review of the patient’s medical and dental histories and clinical findings (Box 5.1). In general, identification of patients with extreme prognoses—either good or hopeless—is reasonably straightforward in comparison with determining a prognosis for patients with prognoses in between. The various guidelines available to predict the future of a tooth with a poor or questionable prognosis are unreliable. Historically, a tooth was considered to have a poor prognosis if it had 50% attachment loss or a class II furcation; a tooth had a questionable prognosis if it had more than 50% attachment loss, a class II or class III furcation, or a poor crown-to-root ratio or poor root form.
The dentist refines the prognosis after observing the response to initial periodontal therapy. Initial therapy includes SC/RP, improvement in oral hygiene, and replacement or recontouring of defective restorations that compromise plaque removal. Initial therapy reduces the bacteria in the sulcus, detoxifies the root surface, and eliminates micro-environments that harbor bacteria, such as calculus and defective restorations. If defective restorations are not corrected as part of initial therapy, the healing response will be stunted. Caries near the gingiva, marginal overhangs, and open contacts should all be corrected before or at the time of SC/RP for optimal gingival healing (Fig. 5.7). In patients who respond to initial therapy with significant reductions in pocket depths and in BOP, the prognosis is significantly more positive.
Time is on the dentist’s side in further evaluation of the overall dentition and of specific teeth. When other problems allow, patients should undergo SPT every 2 to 3 months during the first year after initial phase therapy. All urgent dental needs are addressed, and the patient’s oral hygiene and maintenance compliance are evaluated during this year. The changes recorded in periodontal health are compared to the reevaluation data. This third refinement of prognosis enables much more accurate planning, allowing comprehensive restorative therapy to be initiated at that time.
Teeth with a poor or questionable prognosis can be maintained for many years. Periodontal disease is site specific, and in most instances, a periodontally compromised tooth does not affect the health of adjacent teeth. When possible, the restorative plan can allow such teeth to remain in place, while only teeth or implants with a good or fair prognosis can be used to support a prosthesis to replace missing teeth. It may be possible to maintain the teeth in a periodontally compromised but otherwise intact dentition for an extended period of time. However, if that same patient is missing teeth and now requires comprehensive restorative dentistry, strategic extractions may be necessary to improve prosthetic predictability (Fig. 5.8).
If strategic extractions are indicated, it is advisable to consider whether such teeth can serve as interim abutments (Fig. 5.9) or for implant site development through orthodontic forced eruption (OFE) (Fig. 5.10).44 Both procedures may enhance bone and gingival tissue augmentation. Tooth extraction is always followed by some loss of crestal bone and gingiva (Fig. 5.11). Before the advent of implants, teeth with a hopeless prognosis were simply extracted. In contrast, retention of teeth, even if temporary, can help retain and augment tissue in anticipated implant sites, improving future esthetics and implant considerations.
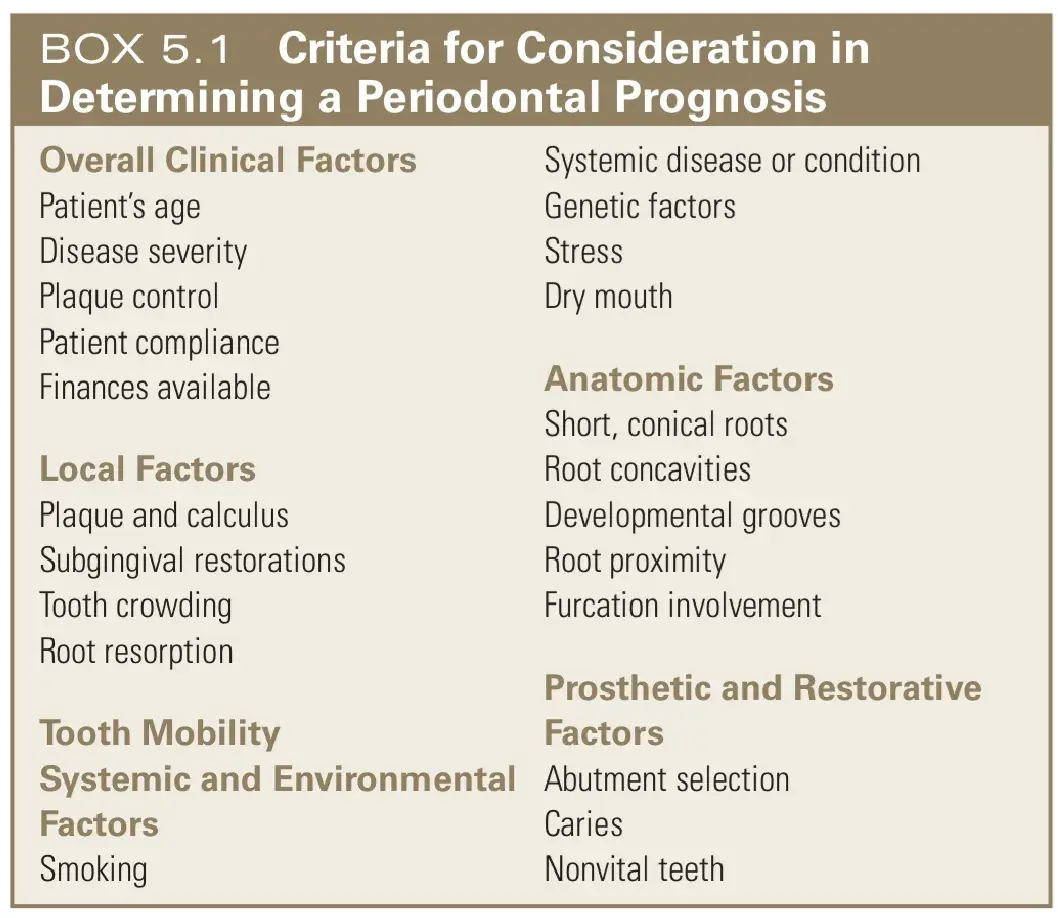
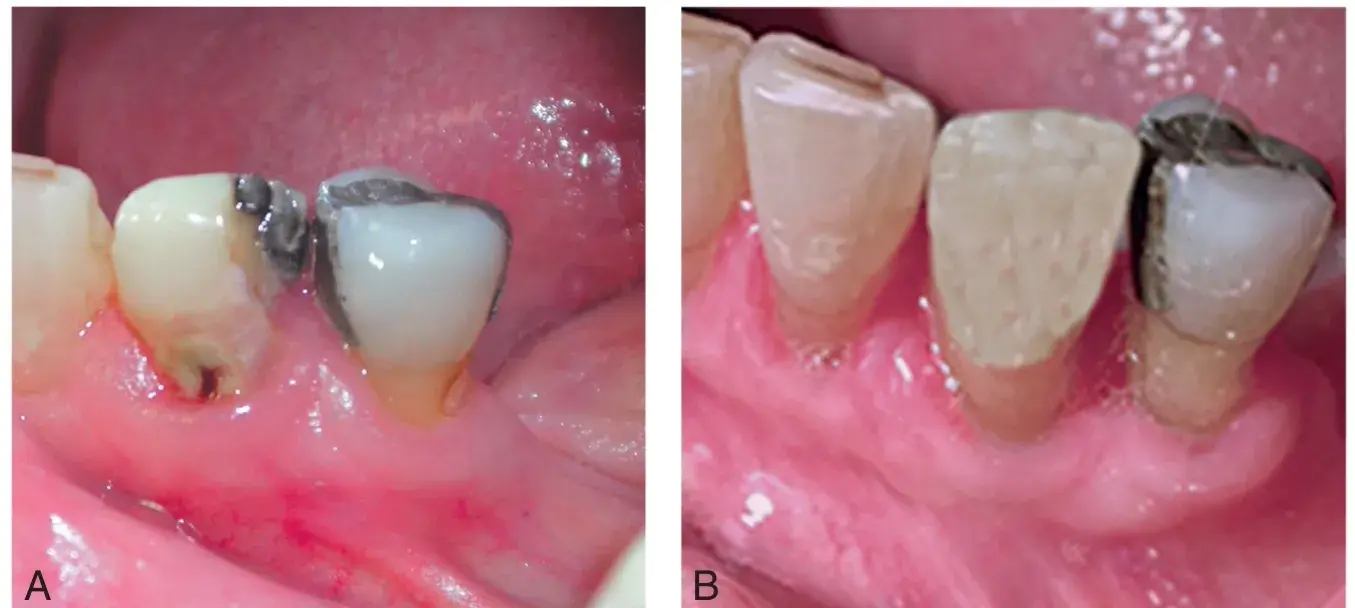 Fig. 5.7 To promote maximum gingival healing after scaling and root planing, open contacts, defective restorations, and dental caries (A) must be corrected (B) during the initial phase of periodontal therapy.
Fig. 5.7 To promote maximum gingival healing after scaling and root planing, open contacts, defective restorations, and dental caries (A) must be corrected (B) during the initial phase of periodontal therapy.
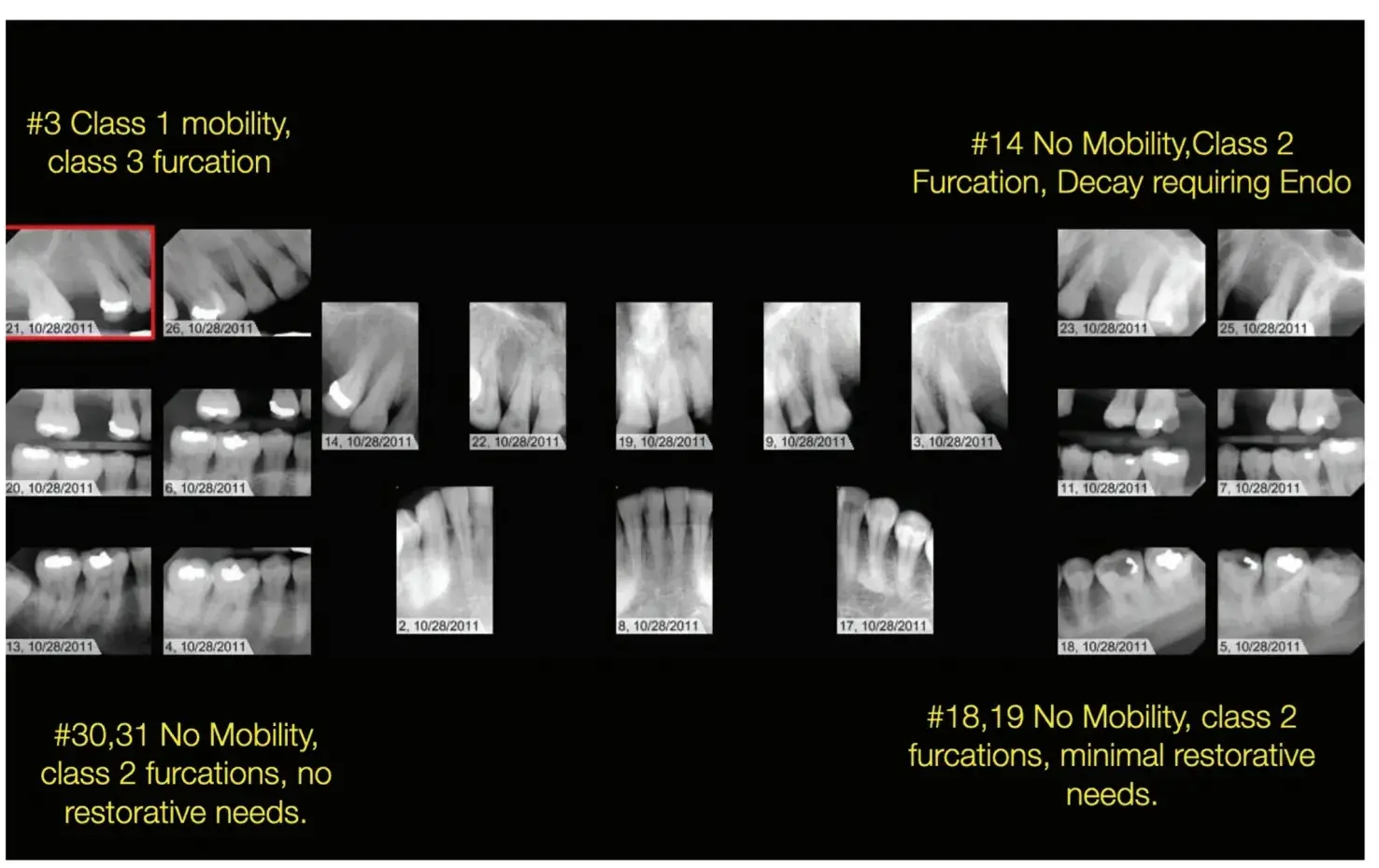 Fig. 5.8 The mandibular arch has an intact dentition with minimal restorative needs, and all teeth should be retained and maintained as long as possible, even with advanced periodontal destruction associated with the molars. The maxillary arch has similar periodontal destruction but now requires extensive restorative treatment and selective extractions are necessary to ensure acceptable longevity of the prostheses.
Fig. 5.8 The mandibular arch has an intact dentition with minimal restorative needs, and all teeth should be retained and maintained as long as possible, even with advanced periodontal destruction associated with the molars. The maxillary arch has similar periodontal destruction but now requires extensive restorative treatment and selective extractions are necessary to ensure acceptable longevity of the prostheses.
 Fig. 5.9 The maxillary right central incisor and maxillary left lateral incisor are used as interim abutments to support a fixed interim restoration that protects the surgical site during healing after the bony augmentation procedure. (From Misch CE. Contemporary Implant Dentistry. 3rd ed. St. Louis: Mosby; 2008.)
Fig. 5.9 The maxillary right central incisor and maxillary left lateral incisor are used as interim abutments to support a fixed interim restoration that protects the surgical site during healing after the bony augmentation procedure. (From Misch CE. Contemporary Implant Dentistry. 3rd ed. St. Louis: Mosby; 2008.)
 Fig. 5.10 A maxillary right central incisor with a hopeless prognosis can be orthodontically forced to erupt to develop additional bone and gingival tissue before extraction. (A) Initial recession. (B) Simulated gingival position after 3 months of orthodontic treatment.
Fig. 5.10 A maxillary right central incisor with a hopeless prognosis can be orthodontically forced to erupt to develop additional bone and gingival tissue before extraction. (A) Initial recession. (B) Simulated gingival position after 3 months of orthodontic treatment.
 Fig. 5.11 Congenital absence of maxillary lateral incisors. (A) The maxillary right central incisor failed and was removed. Note the loss of bone and gingiva (arrow) in the right anterior maxilla, where two adjacent teeth are missing. (B) The bone and gingiva are better preserved (arrow) in the left anterior maxilla, where only a single tooth is missing. The patient had a thin biotype; therefore, gingival and bone changes were severe.
Fig. 5.11 Congenital absence of maxillary lateral incisors. (A) The maxillary right central incisor failed and was removed. Note the loss of bone and gingiva (arrow) in the right anterior maxilla, where two adjacent teeth are missing. (B) The bone and gingiva are better preserved (arrow) in the left anterior maxilla, where only a single tooth is missing. The patient had a thin biotype; therefore, gingival and bone changes were severe.
CONNECTIVE TISSUE
The importance of an abundance of thick, dense connective tissue to the long-term prognosis can no longer be debated.
Decreased gingival inflammation, reduced BOP, and less bone loss have been observed around prosthetically restored natural teeth and implants when dense connective tissue is present. Ideally, 5mm of dense connective tissue of which 3mm is attached should be present (Fig. 5.12). In situations where less connective tissue is present, a gingival augmentation procedure is indicated. The importance of thick, dense connective tissue was recognized in the 60s for natural teeth. However, in the mid-80s, the arrival of the mandibular fixed hybrid implant supported restoration made many question its importance. That unique restoration with its restorative interface placed 3mm above the gingiva and dense, flat and abundant bone, achieved excellent long-term predictability even in cases without dense, thick connective tissue. This led many to question the need for dense connective tissue. As implant prosthodontics evolved and implants were used to replace missing teeth in other areas of the mouth and the restorative interface was placed at the gingival crest, subgingivally, or with less cleansable designs, complications developed. The consensus today recognizes the value of thick, dense connective tissue to protect the alveolar bone whenever the restorative interface will challenge plaque control.
 Fig. 5.12 A minimum of 5mm of keratinized tissue of which 3mm are attached to periosteum are necessary on teeth and implants that are restored with a fixed prosthesis.
Fig. 5.12 A minimum of 5mm of keratinized tissue of which 3mm are attached to periosteum are necessary on teeth and implants that are restored with a fixed prosthesis.
BIOLOGIC WIDTH
The normal gingival attachment consists of nearly 1 mm of a strong connective tissue attachment to the root cementum and about 1 mm of a weaker epithelial adhesion to a clean, smooth surface. The combination of connective tissue attachment and epithelial adhesion is termed biologic width. Two millimeters is the minimum amount of space that the gingiva needs to attach to the root. In health, sulcus depth varies between 1 mm on the facial and lingual aspects and 2 to 3 mm interproximally (Fig. 5.13). These numbers are averages and do not characterize every patient.49 Average values are adequate to understand the concept of biologic width; however, the true biologic width for an individual patient can only truly be determined by establishing gingival health and allowing the biologic width to establish on its own. Probing through the attachment to the bone level and subtracting the sulcus depth to determine the biologic width as advocated by some is unpredictable in areas of thin bone, such as the facial surfaces of most teeth because the rounded end of a periodontal probe may not stop on the bone crest and may glance past.
In patients with thin bone, some suggest the use of a local anesthetic needle with the bevel facing away from the tooth to sound the thin bony crest of anterior teeth.
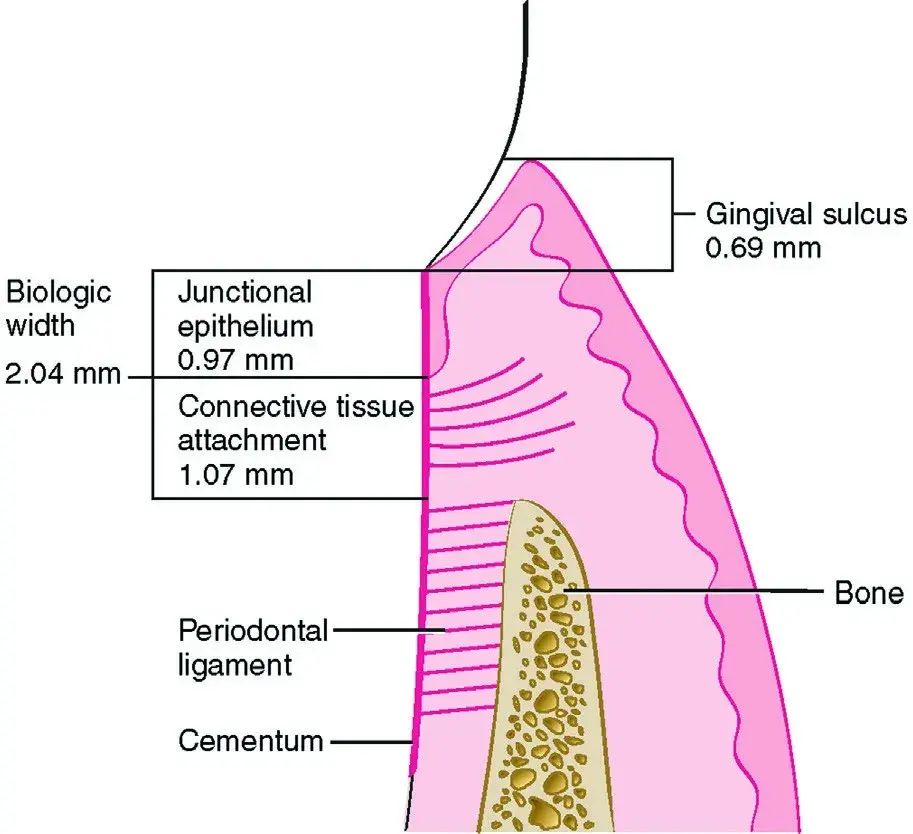 Fig. 5.13 Average values for biologic width. Any encroachment into this 2.04-mm space will result in an inflammatory reaction. (From Newman MG, et al. Carranza's Clinical Periodontology. 10th ed. St. Louis: Saunders; 2006.)
Fig. 5.13 Average values for biologic width. Any encroachment into this 2.04-mm space will result in an inflammatory reaction. (From Newman MG, et al. Carranza's Clinical Periodontology. 10th ed. St. Louis: Saunders; 2006.)
MARGIN PLACEMENT
Preparation finish lines can be supragingivally, equigingivally, or subgingivally, that is intrasulcularly. Supragingival and equigingival margins are easier to prepare, make an impression, and finish to a smooth polished surface. This facilitates effective plaque removal and the maintenance of gingival health. In some circumstances, previous restorations, existing caries, esthetics, or retention and resistance form needs dictate a subgingival margin. In comparison with an intact tooth surface, all restorations exhibit open, rough margins that favor plaque retention. The more supragingival the restoration margin is located, the easier the access for plaque removal, and the healthier the gingival tissue will be.50,51 A toothbrush can clean only 0.5mm subgingivally, floss can clean up to 2.5mm below the gingiva, and a water irrigation device can alter bacterial composition up to 4mm below the gingiva (Fig. 5.14; Table 5.2). The majority of patients rely on toothbrushing as their only form of oral hygiene.
Subgingival margins are problematic and should be avoided when possible. Periodontally, a subgingival margin always results in a gingival inflammatory response. This inflammatory response ranges from a mild, subclinical inflammation to an overt inflammatory response with swelling, redness, tenderness, bleeding, and possibly bone loss. The degree of inflammatory response is determined by many factors. Two of these factors, the patient’s overall systemic health and the patient’s gingival biotype, are beyond a dentist’s control. However, by being aware of the patient’s systemic health and biotype (defined later in the chapter), the dentist can make choices before the decision to place a subgingival restoration. The factors under a dentist’s control include the extent to which the preparation margin is placed farther apically, the quality of the marginal fit, and the smoothness of the subgingivally placed restorative material. Margins that fit in the acceptable range and that are placed in a cleansable area provoke only a mild, subclinical inflammatory response. Margins that are significantly open harbor a large number of bacteria and provoke a larger inflammatory response (Fig. 5.15). Metal, ceramic, and resin margins are equally compatible with gingival health when polished to the same degree of smoothness. The emergence profile of the restoration should follow the tooth anatomy apical to the margin. Gingival health is better maintained if the crown is slightly undercontoured rather than overcontoured (see Chapter 7). Historically the most frequent reason for overcontouring restorations was insufficient tooth reduction, which forces the technician to overbuild the contours.
However, contemporary tooth preparation designs are attempting to preserve more enamel and cervical tooth struction. A general consideration is that a minimum of 3mm of attached dense connective tissue should be present to predict acceptable gingival health when a restorative margin will be placed subgingivally.
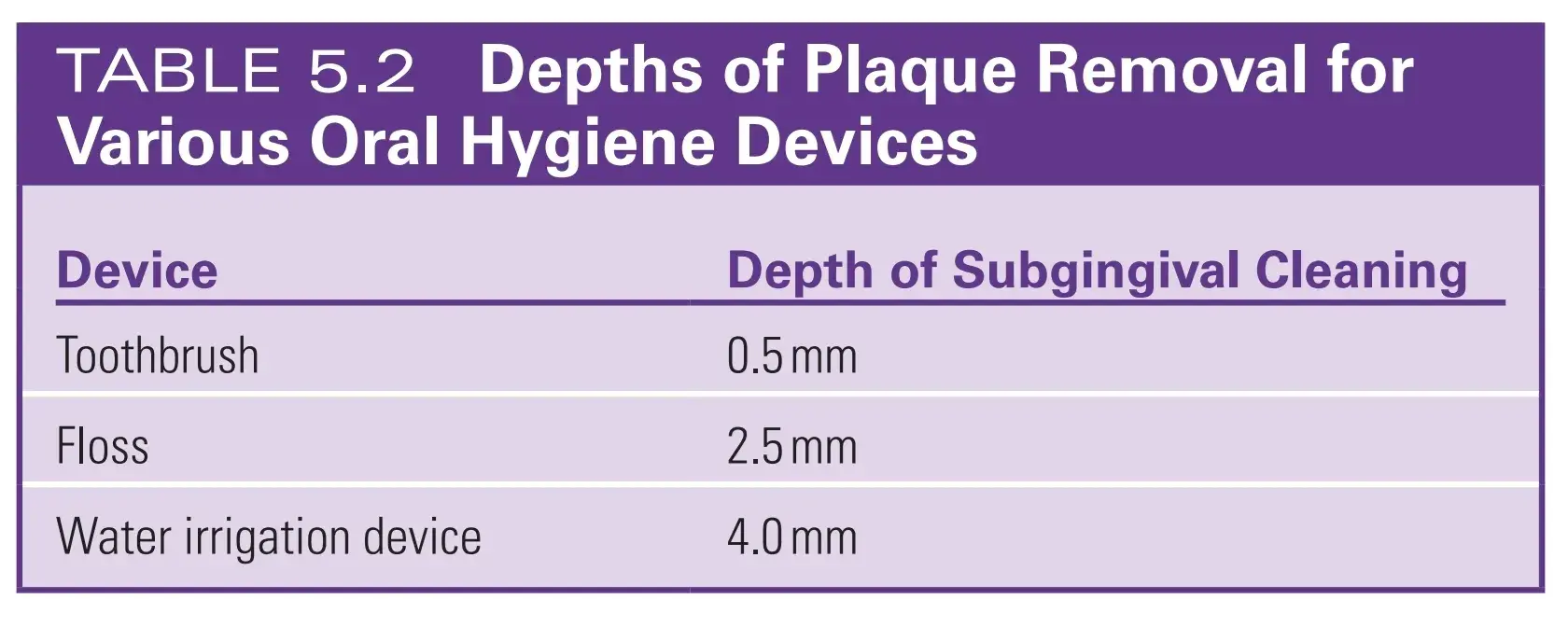
 Fig. 5.14 Depths of plaque removal for various oral hygiene devices. Subgingival irrigation with water or chlorhexidine is more effective in reducing marginal bleeding and bleeding on probing than supragingival rinsing with chlorhexidine (see Table 5.3). (A) The Waterpik Classic Water Flosser. (B) The Waterpik Cordless Water Flosser. (C) Pulsation creates two zones of hydrokinetic activity. (D) Irrigator tips. From left to right: standard jet tip, Pik Pocket subgingival irrigation tip, and cannula. (A and B, Courtesy Water Pik, Inc., Fort Collins, Colorado. C and D, From Newman MG, et al. Carranza's Clinical Periodontology. 10th ed. St. Louis: Saunders; 2006.)
Fig. 5.14 Depths of plaque removal for various oral hygiene devices. Subgingival irrigation with water or chlorhexidine is more effective in reducing marginal bleeding and bleeding on probing than supragingival rinsing with chlorhexidine (see Table 5.3). (A) The Waterpik Classic Water Flosser. (B) The Waterpik Cordless Water Flosser. (C) Pulsation creates two zones of hydrokinetic activity. (D) Irrigator tips. From left to right: standard jet tip, Pik Pocket subgingival irrigation tip, and cannula. (A and B, Courtesy Water Pik, Inc., Fort Collins, Colorado. C and D, From Newman MG, et al. Carranza's Clinical Periodontology. 10th ed. St. Louis: Saunders; 2006.)
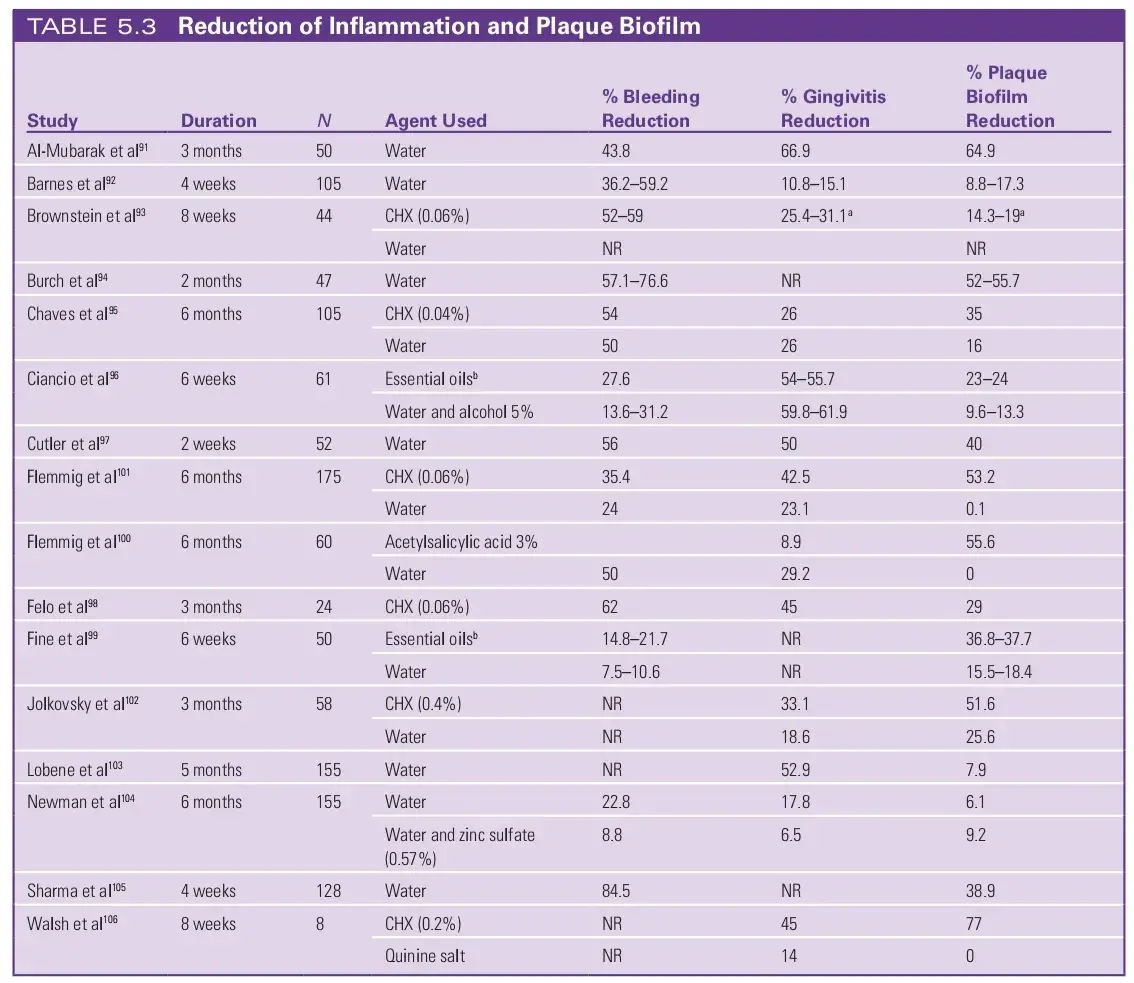
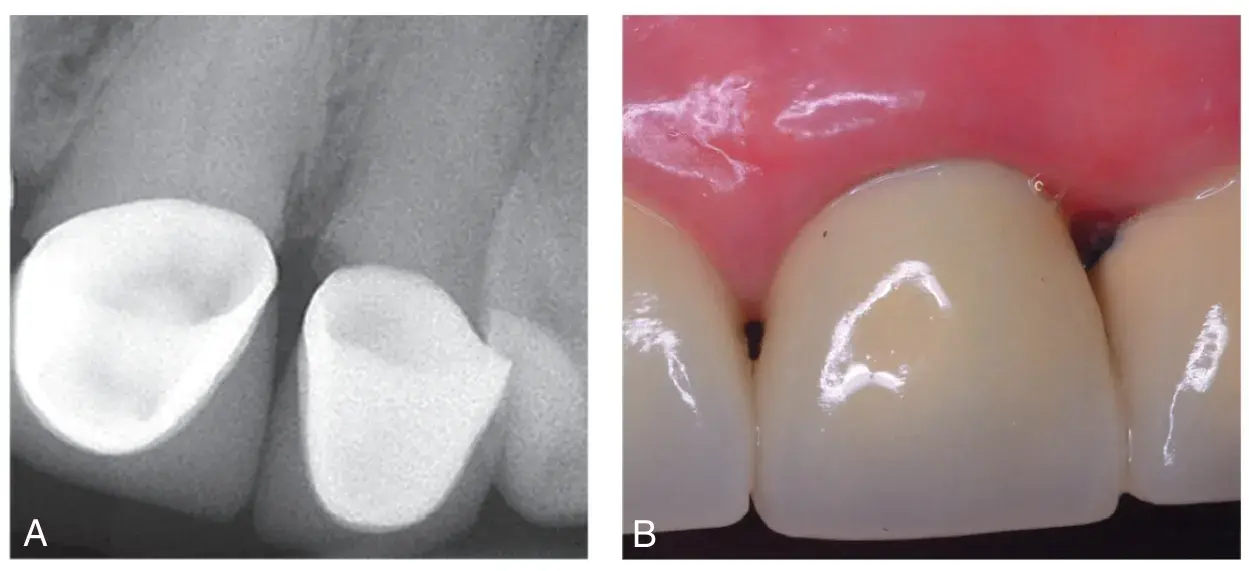 Fig. 5.15 Open margins noted on mesial and distal maxillary left central and lateral incisors result in a significant inflammatory response with bone loss and destruction of the interdental papilla. (A) Radiographs. (B) Appearance.
Fig. 5.15 Open margins noted on mesial and distal maxillary left central and lateral incisors result in a significant inflammatory response with bone loss and destruction of the interdental papilla. (A) Radiographs. (B) Appearance.
Guidelines for Subgingival Margin Placement
A general guideline is that tooth preparation finish lines should not be placed in the periodontal attachment if at all possible. If intrasulcular placement is essential, it should be at no more than half the depth of the gingival sulcus (see Chapter 7). In a healthy periodontal sulcus, the tip of a probe extends approximately 0.5mm into the epithelial attachment. The base of the healthy sulcus is the most coronal portion of the epithelial attachment, and the restorative margin cannot encroach on this attachment. Therefore, if the sulcus probe is 1mm, the restoration cannot extend any more than 0.5mm subgingivally without encroaching upon the attachment (biologic width). A shallow healthy sulcus is also less susceptible to recession than are inflamed periodontal tissues. A 3-mm healthy interproximal sulcus allows the margin to be placed 1.0 to 1.25mm subgingivally. However, the deeper the sulcus, the greater is the potential for gingival recession after any treatment.
Common restorative considerations that dictate placement of margins below the gingiva include (1) creating adequate resistance and retention form, (2) allowing the margin to be placed on sound tooth structure apical to any excavated carious lesion or existing restoration, and (3) masking the tooth/restoration interface in order to mask a color change between the restoration and the tooth. Margins placed deeper than 1mm below the gingival crest create a greater challenge in preparing a smooth margin, obtaining an accurate impression, evaluating the marginal fit of the final restoration, and in removal of residual cement; these difficulties will hinder future plaque removal and logically result in increased gingival inflammation (Fig. 5.16).
Tooth preparation finish lines that are within the attachment create an inflammatory response. Some in the field of dentistry coin the inflammatory response as a biologic width violation (BWV). The response to crown margin placed within the periodontal attachment is a function of the bone thickness. Sites with thin bone may exhibit bone loss due to the inflammatory process. Sites with thick bone most often result in a chronic inflammation without bone loss. Biological with violations frequently occur at the mesiofacial or the distofacial line angles of maxillary anterior teeth treated with fixed restorations and in the posterior proximal sites due to caries extension.
 Fig. 5.16 (A) Note the dark discoloration of the teeth and roots. The maxillary left lateral incisor will be extracted and the canine requires endodontic treatment and a post-and-core before a three unit fixed partial denture is fabricated. (B) The restorative margins on the premolar and canine were placed at the gingival crest and elicited no visual evidence of inflammation. The restorative margin on the central incisor was placed subgingivally to cover the dark root and elicited a visible inflammatory response.
Fig. 5.16 (A) Note the dark discoloration of the teeth and roots. The maxillary left lateral incisor will be extracted and the canine requires endodontic treatment and a post-and-core before a three unit fixed partial denture is fabricated. (B) The restorative margins on the premolar and canine were placed at the gingival crest and elicited no visual evidence of inflammation. The restorative margin on the central incisor was placed subgingivally to cover the dark root and elicited a visible inflammatory response.
Gingival Biotype/Phenotype
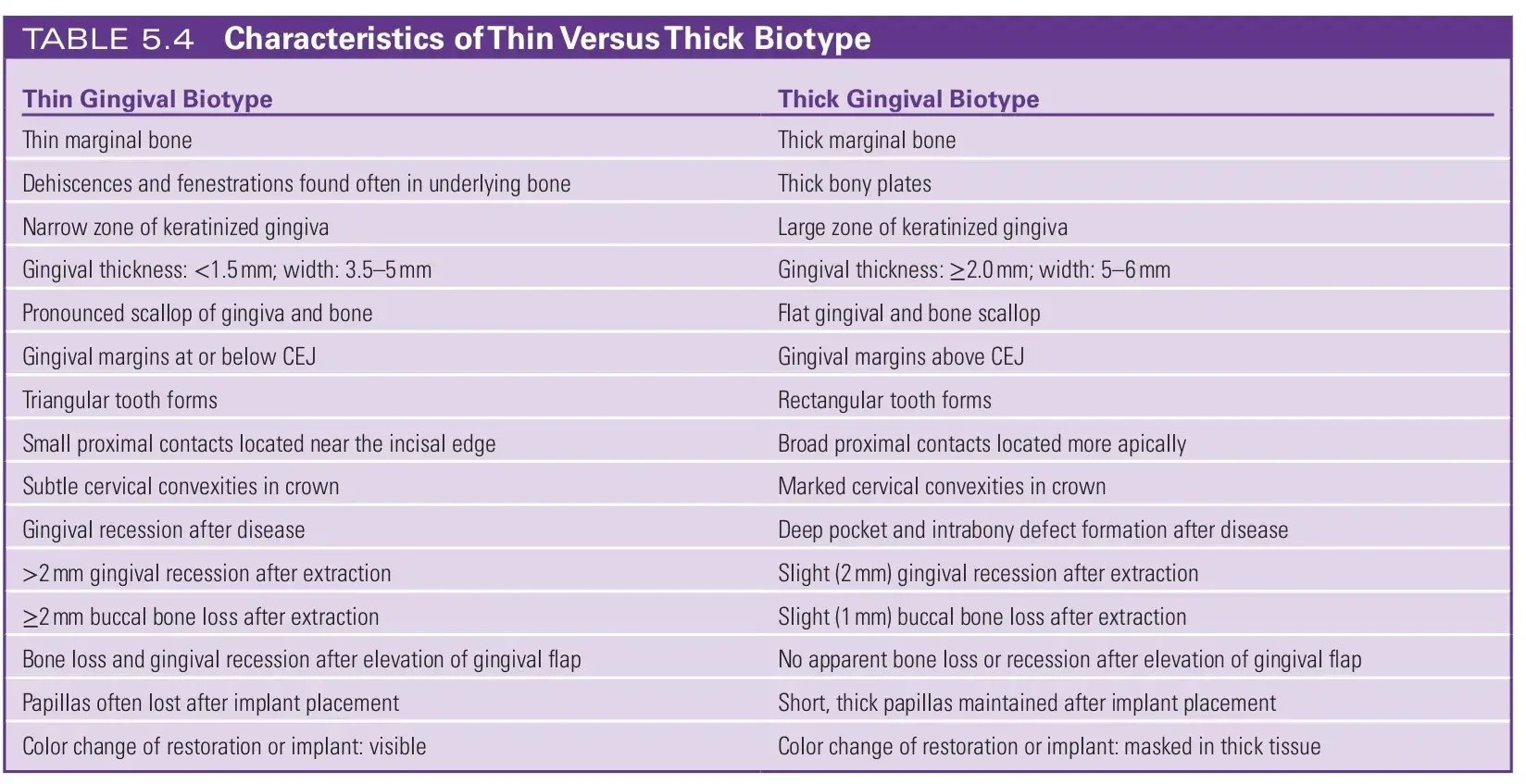
Responses to biologic width invasion vary by different gingival biotypes. In the field of genetics, the characteristics one portrays as the result of the interactions of their genotype with their environment is known as their phenotype. In the field of dentistry biotype is commonly used instead of phenotype; however, the scientific correctness of the term biotype has been debated.
A combination of thin bone with thin gingiva overlying the bone is termed a thin biotype.60 The inflammatory response results in swelling, edema, redness, and bleeding, but in thin biotypes, gingival recession and bone loss occur and a new biologic width is established at a more apical level. A thick gingival biotype characterizes two thirds of the population, and most people with a thick biotype are men (Fig. 5.17). A thin gingival biotype is most often found in women. Thin and thick gingival biotypes can exist within the same dentition.
If a probe is placed within the gingival sulcus, and if the biotype is thin, the tip of the probe can be seen through the sulcus. Patients with thin gingival biotypes are at high risk for gingival recession during any dental procedures (Table 5.4).
 Fig. 5.17 (A) Thick biotype. (B) Thin biotype. Note the minimal amount of keratinized tissue and readily visible blood vessels in the patient with the thin biotype.
Fig. 5.17 (A) Thick biotype. (B) Thin biotype. Note the minimal amount of keratinized tissue and readily visible blood vessels in the patient with the thin biotype.
Correcting or Preventing Biologic Width Violations
BWVs can be corrected either by traditional crown lengthening (TCL) with surgical removal of bone from below the restorative margin and movement of the attachment apically (Fig. 5.18),63 by orthodontic extrusion of the tooth (and preparation finish lines) coronally away from the attachment (Fig. 5.19) or by biologic shaping (BS) of the root and tooth during which the existing margin is removed and root anatomy that compromises future plaque removal is eliminated during the surgical procedure.
In earlier editions, we discussed traditional surgical crown lengthening. Crown lengthening is a surgical procedure aimed at exposing more tooth structure for restorative and/or esthetic reasons. Most often this is performed by surgical removal of supporting bone (ostectomy) with concurrent contouring of the adjacent alveolar bone (osteoplasty). The objective is to provide adequate coronal tooth structure to allow retention and resistance for a predicable fixed restoration. Correction of a biologic width invasion uses the previous margin as the reference point from which to create 3 to 5mm of space apically to result in a new and sustainable biologic width. TCL requires aggressive removal of supporting bone, increases the crown to root ratio, and often exposes root anatomy that can make future plaque removal challenging.
The resulting gingival position is reasonably stable at 4 months, and new margins can then successfully be placed. In the anterior region, it is advisable to wait 6 months before final margin placement because of the increased esthetic demands.
Surgical crown lengthening is seldom performed on a single tooth. Bone correction (i.e., recontouring) must be gradual and not result in any abrupt change of direction. Most often, bone must be removed around three adjacent teeth to correct a single biological width violation. In the anterior esthetic zone, surgery is often contraindicated unless all teeth would benefit from a longer tooth length (Fig. 5.20). In the past, in posterior quadrants, surgical crown lengthening has been the treatment of choice. Posterior teeth most often demonstrate retention and/or resistance challenges because of short clinical crowns.
Frequently, existing restorations with subgingival margins are present. Surgical correction through crown lengthening moves margins from a subgingival position to a crestal or supragingival position, where plaque removal is more straightforward. Lasers and closed surgical techniques have been introduced for selected anterior crown lengthening. Keratinized tissue must be adequate for a gingivectomy to be performed yet have 5mm of keratinize tissue remaining. The bone is removed through the sulcus with hand instruments, rotary instruments, or lasers to reestablish a healthy biologic width 3mm below the restorative margin. This novel minimally invasive approach is very technique-sensitive. The resultant root surface is rougher, and troughs are created in thicker bone. Clinically, these findings should be approached with caution, but they do not significantly alter the short-term outcomes in comparison to a TCL approach in carefully selected anterior teeth.
 Fig. 5.18 Surgical correction of biologic width violations: interproximal mandibular right second premolar and first molar. (A and B) Initial clinical views. (C) Interim restoration in place before surgery. (D) Short preparations and a lack of ferrule. (E) Immediately after crown lengthening. (F) Definitive restorations placed.
Fig. 5.18 Surgical correction of biologic width violations: interproximal mandibular right second premolar and first molar. (A and B) Initial clinical views. (C) Interim restoration in place before surgery. (D) Short preparations and a lack of ferrule. (E) Immediately after crown lengthening. (F) Definitive restorations placed.
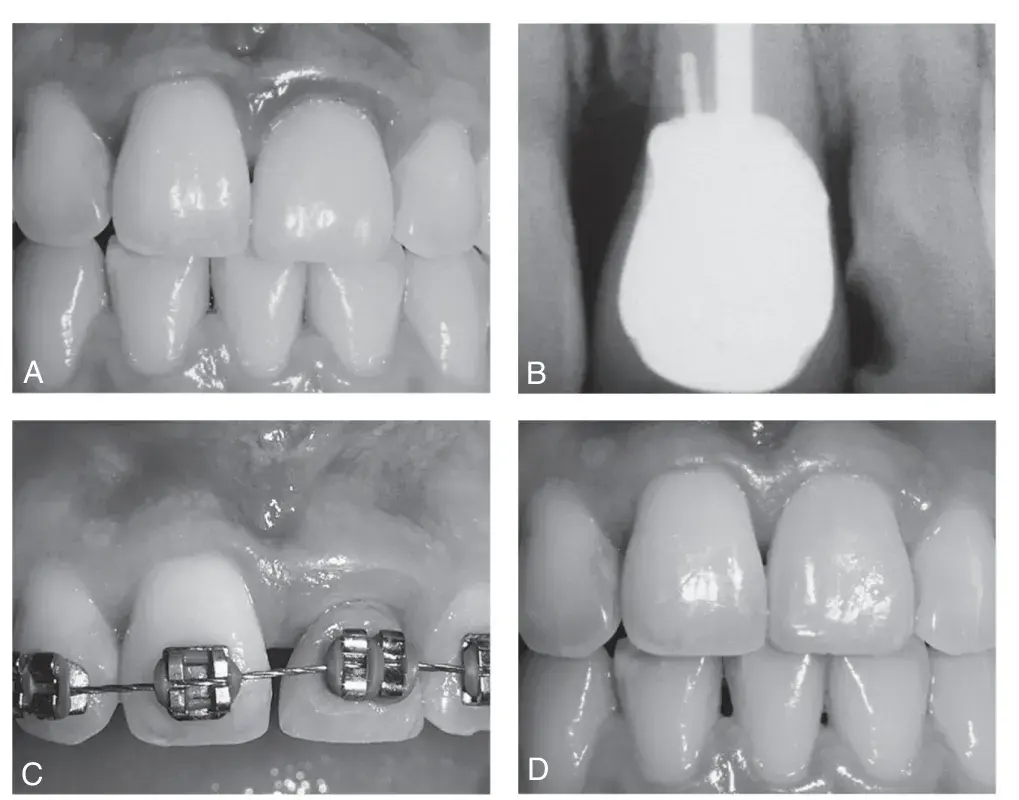 Fig. 5.19 Orthodontic correction of a biologic width violation (BWV). (A) Tooth #9 exhibits red, edematous gingiva adjacent to new crown. (B) Bite-wing radiograph confirms BWV. (C) Orthodontic treatment is utilized to pull gingiva and bone incisally. (D) Surgical removal of newly gained gingiva and bone results in correction of BWV and preservation of gingival esthetics. (From Newman MG, et al. Carranza's Clinical Periodontology. 10th ed. St. Louis: Saunders; 2006.)
Fig. 5.19 Orthodontic correction of a biologic width violation (BWV). (A) Tooth #9 exhibits red, edematous gingiva adjacent to new crown. (B) Bite-wing radiograph confirms BWV. (C) Orthodontic treatment is utilized to pull gingiva and bone incisally. (D) Surgical removal of newly gained gingiva and bone results in correction of BWV and preservation of gingival esthetics. (From Newman MG, et al. Carranza's Clinical Periodontology. 10th ed. St. Louis: Saunders; 2006.)
 Fig. 5.20 (A) Maxillary right central incisor has fractured at the gingiva. (B) Surgical crown lengthening would necessitate removal of gingiva and bone around all three adjacent teeth (indicated by curved white line). (C) The result would be longer, uneven teeth.
Fig. 5.20 (A) Maxillary right central incisor has fractured at the gingiva. (B) Surgical crown lengthening would necessitate removal of gingiva and bone around all three adjacent teeth (indicated by curved white line). (C) The result would be longer, uneven teeth.
BIOLOGIC SHAPING
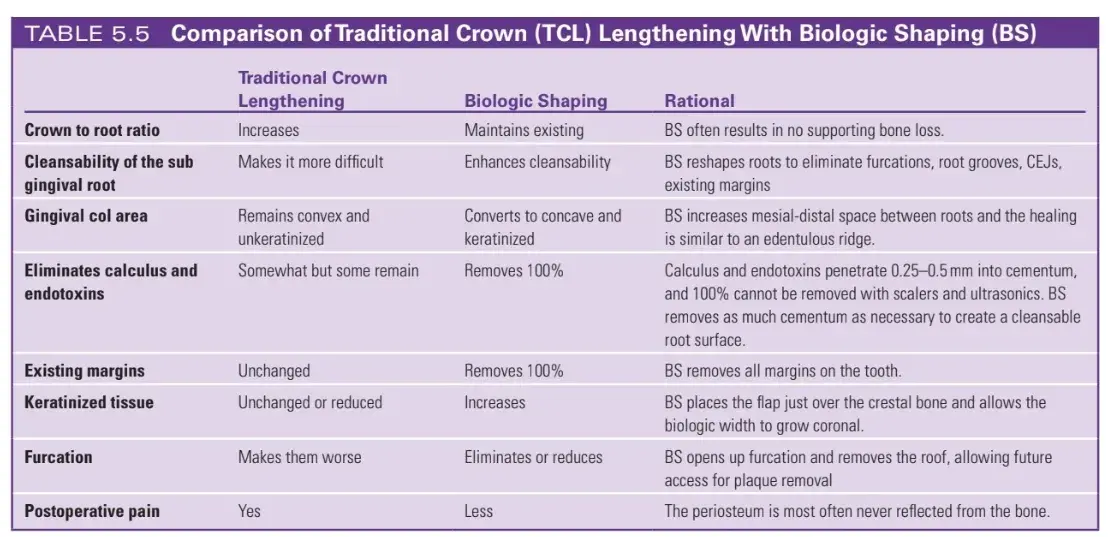
Biologic shaping (BS) in an alternative to traditional surgical crown lengthening (Figs. 5.21–5.50). Dr. Melker coined the term BS over 35 years ago to describe an improved concept. The procedure is much more conservative to the supporting alveolar bone. It removes the existing margins and contours the root, eliminating much of the root concavities, furcations, root grooves, and enamel projections that compromise long term maintenance of gingival health. The biologic width is allowed to reestablish with minimal or no removal of supporting bone.
The restorative dentist is then able to place margins supragingival and facilitate the greatest gingival health (Table 5.5). BS begins with removal of all existing carious lesions, placing a solid bonded resin foundation restoration and preparing the tooth for an interim crown. The interim crown margins should be feather edge. The surgeon removes the interim restoration and reflects a partial thickness envelope flap on the buccal surface, when possible. In areas with tori or exostosis, a full thickness flap is required. The lingual flap is a full thickness flap. Buccal and lingual flaps are extended at least one tooth mesial and distal to the tooth or area in question. The tooth is examined for anatomy that will compromise future cleansability such as furcations, root grooves, enamel projections, and existing margins that violate the biologic width. The alveolar bone is examined for excess bone that creates bulky contours that prevent smooth gingival contours. The surgeon then formulates a plan and shapes the root and crown to eliminate the existing margins and minimizes any contours that will affect future cleansability (see Fig. 5.21). The non-supporting bone is then shaped to create smooth, parabolic architecture. Finally, if necessary, the supporting bone is shaped as conservatively as possible to create the crown length necessary for the definitive restoration. The margins of the previous restorations are completely removed during this process. The periosteal layer is not reflected from the underlying bone in most situations.
The overlying gingival flap and the root are evaluated, any areas with bone dehiscences or less than 5mm of dense connective tissue are augmented with a connective tissue graft sutured between the periosteum and the overlying gingival flap. The gingival flap is sutured at the junction of the root and the osseous crest (see Figs. 5.31 and 5.32). Exposed dentinal surfaces are treated with desensitizing medications after which the interim restorations are modified to ensure all margins are supragingival by at least 2mm and are recemented. The restorative dentist replaces the interim restorations in 4 weeks; however, no new preparation margins are created at this time. The new interim restoration is placed 1 to 2mm supragingivally. The surgical site is allowed to reestablish a healthy biologic width, and at approximately 4 months light chamfer margins are placed just slightly supragingivally (see Figs. 5.33 and 5.34) after which the restorations are completed (see Fig. 5.35). It is imperative that the contours of the restorations follow the contours established by the root anatomy.
BS has many advantages over conventional crown lengthening. It requires less removal of supporting bone than the more common TCL. Placement of the gingival flap at the junction of the root and alveolar bone and supragingivally interim restorations allow the healing process to develop a stable biologic width with minimal sulcus. Conventional surgical crown lengthening increases the crown/root ratio and results in a greater loss of gingiva and bone from adjacent teeth. The root anatomy of posterior teeth become much more irregular as they move apically. Conventional surgical crown lengthening removes bone but does not change the root profile. BS alters the root surface to eliminate or greatly reduce the irregularities and concavities. Normal interproximal anatomy consists of a buccal and lingual papilla connected by an un-keratinized gingival col. Bacterial invasion through this un-keratinized col is one of the etiologic factors in the development of an initial periodontal infection. BS increases the mesio-distal space between adjacent teeth. As a result the gingival tissue heals in the same manner as an edentulous ridge with a convex shape that is covered with a dense connective tissue. Well executed BS should allow the patient to easily clean the tooth with a toothbrush and dental floss and provide similarly improved access to a dental hygienist’s instruments.
The disadvantages of BS are few. It is a significant improvement compared with TCL but requires close coordination between highly skilled restorative and surgical team members.
Hundreds of treated patients with over 35 years of survival have been documented of teeth that most dentists would have likely extracted and restored with an implant. However, with dental implants, long term maintenance issues remain a concern.
Treating peri-implantitis, screw fractures or loosening, and other complications can be costly to the patient and the dental team. Our first priority should be keeping the natural tooth for as long as possible, and BS is one of the options to do so. Surgical guides can be fabricated from a traditional hand waxed diagnostic cast or utilizing digital technology. These guides can be very helpful conveying the desired location for the gingival margin. The resolution of cone beam computed tomography is not accurate enough to reliably demonstrate the thin bone on the facial surfaces of dental roots. Reflection of a gingival flap is necessary to successfully evaluate and treat biologic width problems. A surgical guide is a tool that conveys the desired location of the gingival margin, but it is the skill and knowledge of the dentist directly visualizing the bone, root anatomy, position of the cementoenamel junction (CEJ), thickness of the connective tissue and other factors that create the final desired result.
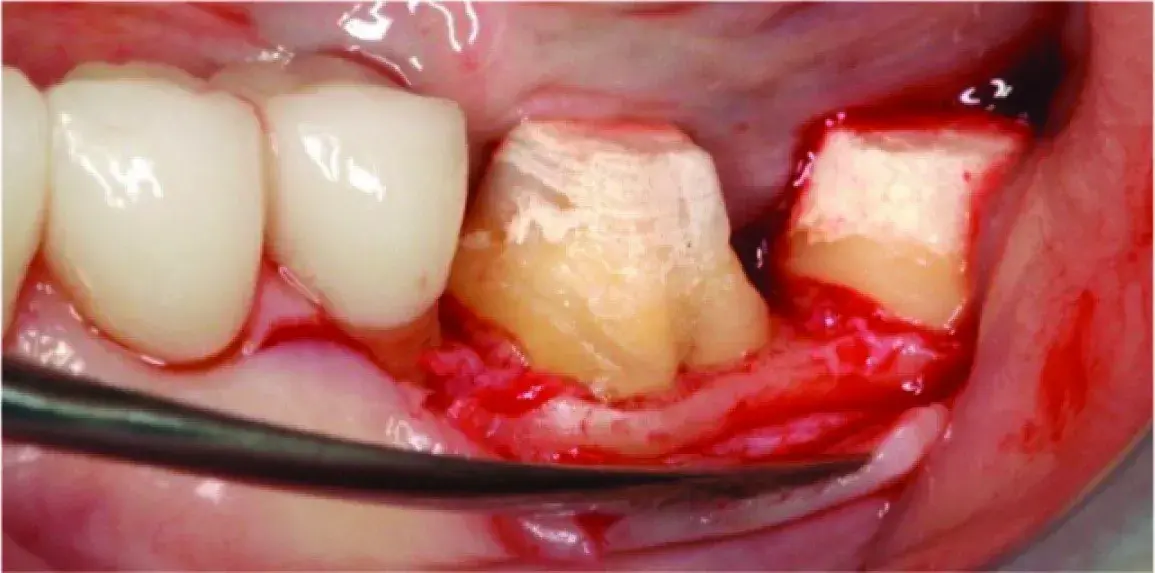 Fig. 5.21 Right mandibular first molar. The previous fixed restoration margin created a roof to the furcation exacerbating if not causing the periodontal problem. Traditional crown lengthening would have removed 2 to 3mm of additional supporting bone and made the situation even worse.
Fig. 5.21 Right mandibular first molar. The previous fixed restoration margin created a roof to the furcation exacerbating if not causing the periodontal problem. Traditional crown lengthening would have removed 2 to 3mm of additional supporting bone and made the situation even worse.
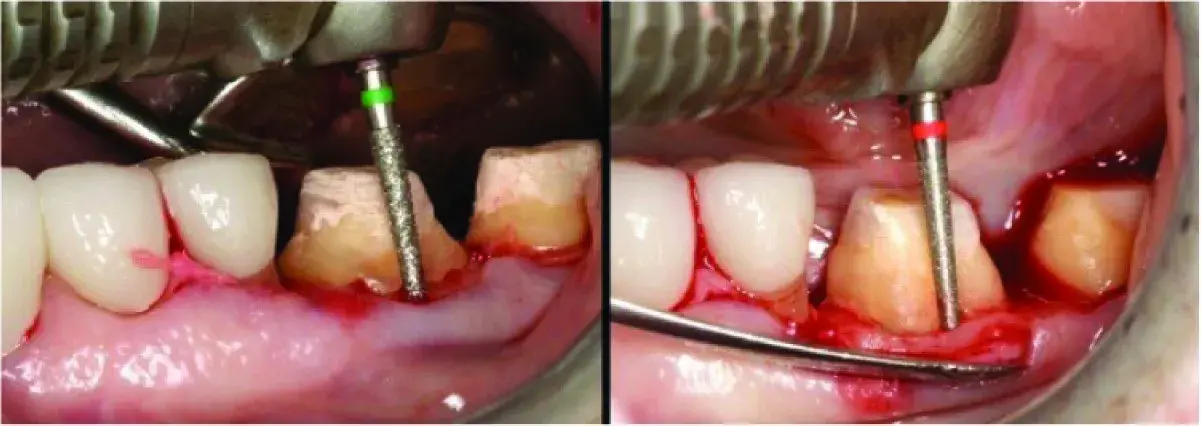 Fig. 5.22 (A) Biologic shaping (BS) removes all the existing margins AND removes roof of class I furcation, making it cleansable. A class II furcation can often be changed into a class I or better. (B) Medium and then fine grit diamond rotary instruments are used to remove all previous margins from the tooth.
Fig. 5.22 (A) Biologic shaping (BS) removes all the existing margins AND removes roof of class I furcation, making it cleansable. A class II furcation can often be changed into a class I or better. (B) Medium and then fine grit diamond rotary instruments are used to remove all previous margins from the tooth.
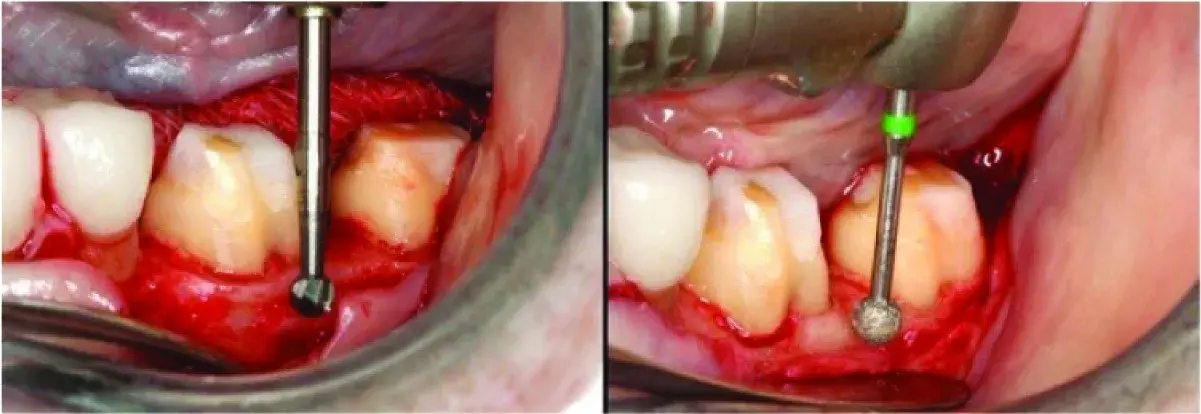 Fig. 5.23 (A) Nonsupporting bone shaped (osteoplasty) to improve gingival contours. Crown-to-root ratio is unchanged. The buccal flap is a split thickness flap and the periosteum is reflected only enough to allow access for the necessary osteoplasty. (B) The bone is shaped to allow smooth parabolic contours.
Fig. 5.23 (A) Nonsupporting bone shaped (osteoplasty) to improve gingival contours. Crown-to-root ratio is unchanged. The buccal flap is a split thickness flap and the periosteum is reflected only enough to allow access for the necessary osteoplasty. (B) The bone is shaped to allow smooth parabolic contours.
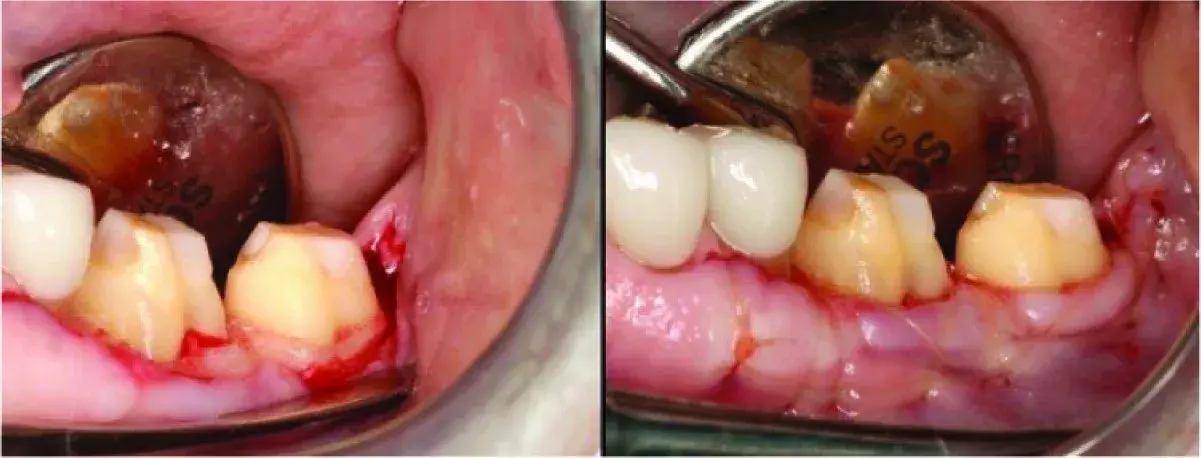 Fig. 5.24 (A) The roof of the furcation has been removed and the definitive restoration can be placed 0.5mm supragingivally for cleansability. (B) The buccal flap split thickness leaves the periosteum intact to protect the bone, minimize postoperative pain, and allow the facial flap to be precisely sutured to the fixed periosteum just occlusally to the crestal bone.
Fig. 5.24 (A) The roof of the furcation has been removed and the definitive restoration can be placed 0.5mm supragingivally for cleansability. (B) The buccal flap split thickness leaves the periosteum intact to protect the bone, minimize postoperative pain, and allow the facial flap to be precisely sutured to the fixed periosteum just occlusally to the crestal bone.
 Fig. 5.25 (A) Biologic shaping is accomplished on all four sides of the tooth, leaving smooth contours that can be cleaned by the patient and dental hygienist. The interim restoration is shortened 2mm occlusally to the sutured gingiva and recemented. This allows the biologic width to reestablish on the biologically shaped and cleaned root and additional keratinized gingiva is gained. Desensitizing and antibacterial medications are applied to the exposed dentin for 4 weeks. The dentist then relines the interim restorations 1mm occlusally to the healing gingiva and allows an additional 8 weeks of healing before placing lite margins 0.5mm supragingivally and making a definitive impression. (B) The contours of the definitive restoration must match the contours of the tooth.
Fig. 5.25 (A) Biologic shaping is accomplished on all four sides of the tooth, leaving smooth contours that can be cleaned by the patient and dental hygienist. The interim restoration is shortened 2mm occlusally to the sutured gingiva and recemented. This allows the biologic width to reestablish on the biologically shaped and cleaned root and additional keratinized gingiva is gained. Desensitizing and antibacterial medications are applied to the exposed dentin for 4 weeks. The dentist then relines the interim restorations 1mm occlusally to the healing gingiva and allows an additional 8 weeks of healing before placing lite margins 0.5mm supragingivally and making a definitive impression. (B) The contours of the definitive restoration must match the contours of the tooth.
 Fig. 5.26 Biologic shaping eliminated the class 1 furcation, allowed the margin to be placed supragingivally, and maintained 100% of the supporting bone and gingiva. Note how the furcation contours are mimics in the definitive crown on the entire buccal surface.
Fig. 5.26 Biologic shaping eliminated the class 1 furcation, allowed the margin to be placed supragingivally, and maintained 100% of the supporting bone and gingiva. Note how the furcation contours are mimics in the definitive crown on the entire buccal surface.
 Fig. 5.27 Buccal cusps on endodontically treated mandibular right 1st molar fractured almost at the level of the facial bone crest. Interim restoration has been placed.
Fig. 5.27 Buccal cusps on endodontically treated mandibular right 1st molar fractured almost at the level of the facial bone crest. Interim restoration has been placed.
 Fig. 5.28 Removal of interim restoration reveals severely compromised tooth.
Fig. 5.28 Removal of interim restoration reveals severely compromised tooth.
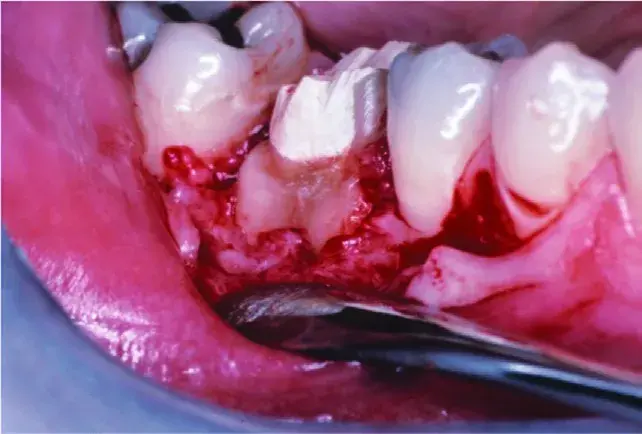 Fig. 5.29 Fracture extends almost to bone crest on mesial buccal root and a class 2 buccal furcation
Fig. 5.29 Fracture extends almost to bone crest on mesial buccal root and a class 2 buccal furcation
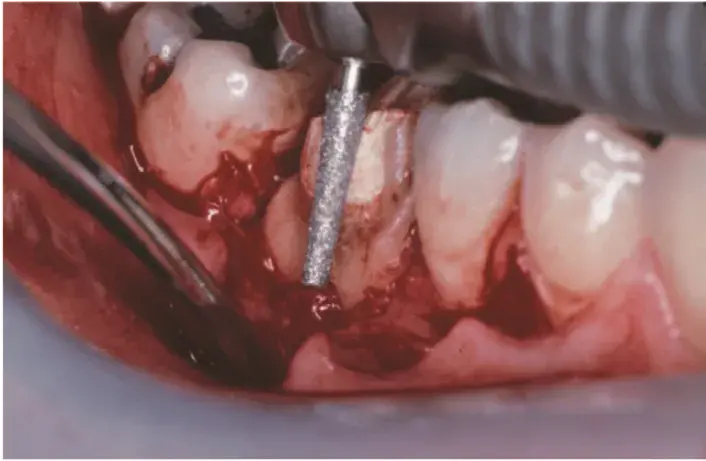 Fig. 5.30 Shaping of the root and crown started with a course grit diamond rotary instrument.
Fig. 5.30 Shaping of the root and crown started with a course grit diamond rotary instrument.
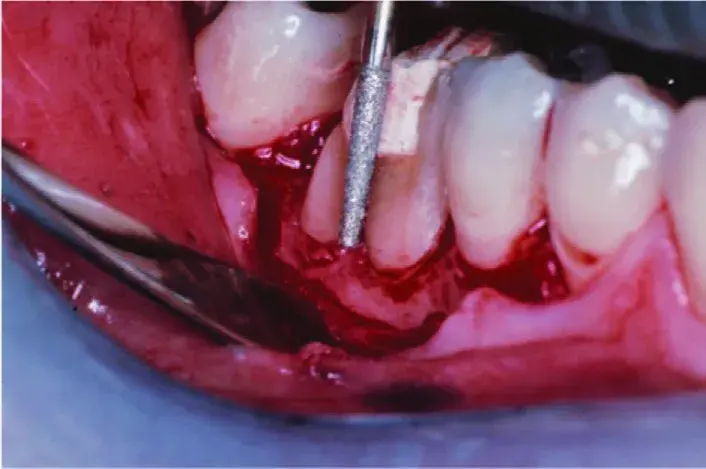 Fig. 5.31 The roof of the furcation is removed.
Fig. 5.31 The roof of the furcation is removed.
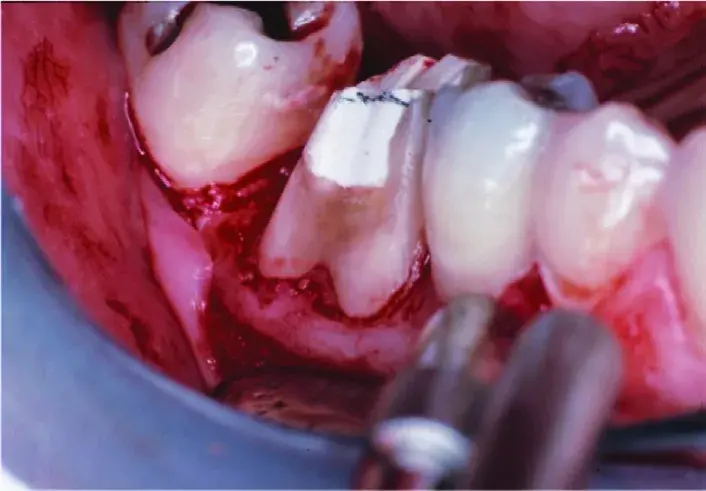 Fig. 5.32 The furcation has been totally eliminated as have all existing margins. Almost no bone has been removed.
Fig. 5.32 The furcation has been totally eliminated as have all existing margins. Almost no bone has been removed.
 Fig. 5.33 Margins on definitive restoration are supragingival; the gingiva has maintained its initial position. The crown contours mimic the shape of the tooth preparation. There is no horizontal probing depth into a furcation.
Fig. 5.33 Margins on definitive restoration are supragingival; the gingiva has maintained its initial position. The crown contours mimic the shape of the tooth preparation. There is no horizontal probing depth into a furcation.
 Fig. 5.34 The buccal sulcus depth is 1mm with pressure firm enough to blanch the tissue.
Fig. 5.34 The buccal sulcus depth is 1mm with pressure firm enough to blanch the tissue.
 Fig. 5.35 Occlusal view of extensively damaged teeth in the maxillary left posterior quadrant before caries removal.
Fig. 5.35 Occlusal view of extensively damaged teeth in the maxillary left posterior quadrant before caries removal.
 Fig. 5.36 Occlusal view of extensively damaged teeth in the maxillary left posterior quadrant before caries removal.
Fig. 5.36 Occlusal view of extensively damaged teeth in the maxillary left posterior quadrant before caries removal.
 Fig. 5.37 Removal of existing restorations and caries. Pulp exposure on the second molar required endodontic treatment.
Fig. 5.37 Removal of existing restorations and caries. Pulp exposure on the second molar required endodontic treatment.
 Fig. 5.38 Minimal remaining tooth structure.
Fig. 5.38 Minimal remaining tooth structure.
 Fig. 5.39 Bonded resin foundation restoration has been placed and prepared with a feather-edge margin.
Fig. 5.39 Bonded resin foundation restoration has been placed and prepared with a feather-edge margin.
 Fig. 5.40 Note the minimal ferrule.
Fig. 5.40 Note the minimal ferrule.
 Fig. 5.41 Caries removed, bonded resin foundation, interim restorations are cemented with polycarboxylate cement. Ready for biologic shaping.
Fig. 5.41 Caries removed, bonded resin foundation, interim restorations are cemented with polycarboxylate cement. Ready for biologic shaping.
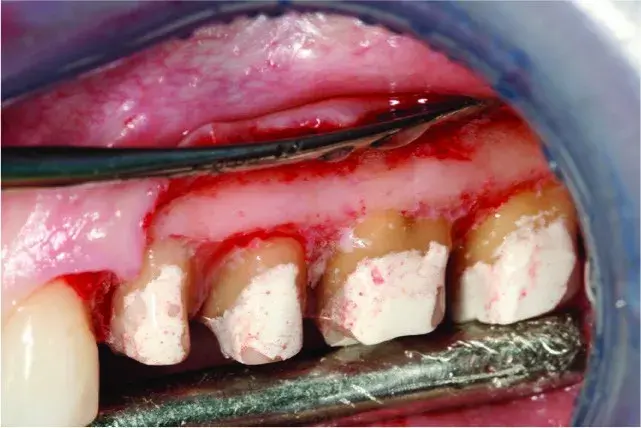 Fig. 5.42 A split thickness flap is reflected.
Fig. 5.42 A split thickness flap is reflected.
 Fig. 5.43 Minor supporting bone removal (ostectomy), mostly reshaping the roots and osteoplasty. Scaling and root planing during surgery does not remove 100% of calculus and endotoxins, but the shaping of the entire root during biologic shaping does. The areas with bleeding are the only places supporting bone has been removed.
Fig. 5.43 Minor supporting bone removal (ostectomy), mostly reshaping the roots and osteoplasty. Scaling and root planing during surgery does not remove 100% of calculus and endotoxins, but the shaping of the entire root during biologic shaping does. The areas with bleeding are the only places supporting bone has been removed.
 Fig. 5.44 The flaps have been sutured to the periosteum just occlusally to the bone crest. The biologic width was allowed to reestablish itself over the next 3 to 4 months of healing because of the supragingival margins on the interim restorations.
Fig. 5.44 The flaps have been sutured to the periosteum just occlusally to the bone crest. The biologic width was allowed to reestablish itself over the next 3 to 4 months of healing because of the supragingival margins on the interim restorations.
 Fig. 5.45 The mesial root concavity on the first premolar has been eliminated, facilitating access to the area for cleaning.
Fig. 5.45 The mesial root concavity on the first premolar has been eliminated, facilitating access to the area for cleaning.
 Fig. 5.46 Note the convex keratinized interproximal gingiva instead of the previous non-keratinized concave gingival col.
Fig. 5.46 Note the convex keratinized interproximal gingiva instead of the previous non-keratinized concave gingival col.
 Fig. 5.47 Chamfer margins have been placed 0.5-mm supragingivally, facilitating impression making and not compromising the periodontal health.
Fig. 5.47 Chamfer margins have been placed 0.5-mm supragingivally, facilitating impression making and not compromising the periodontal health.
 Fig. 5.48 Ideal gingival health and adequate tooth structure and ferrule for long term prosthetic predictability.
Fig. 5.48 Ideal gingival health and adequate tooth structure and ferrule for long term prosthetic predictability.
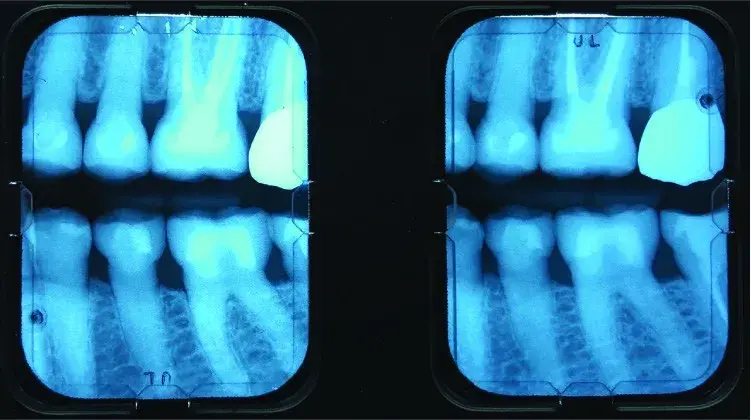 Fig. 5.49 Radiographic image. Excellent restorative margins and abundant supporting bone for long term stability.
Fig. 5.49 Radiographic image. Excellent restorative margins and abundant supporting bone for long term stability.
 Fig. 5.50 Note the excellent gingival health and esthetics in the definitive restorations. Traditional crown lengthening would have resulted in long crowns and exposure of the furcations
Fig. 5.50 Note the excellent gingival health and esthetics in the definitive restorations. Traditional crown lengthening would have resulted in long crowns and exposure of the furcations
PAPILLA
The ideal interdental gingival papilla fills the interproximal embrasure created by (1) the lateral walls of adjacent teeth, (2) coronally by the base of the interproximal contact, and (3) apically by the coronal aspect of the attachment. The clinician can change #1 and #2 with restorative dentistry, orthodontics, or both. The tip of the papilla will extend 5mm above the level of the interproximal bone (3mm above the attachment) when the interproximal embrasure is ideal. Spear and Clooney have suggested “… viewing the papilla as a balloon of a certain volume sitting on the attachment. The balloon of tissue has a form and height dictated by the gingival embrasure of the teeth. With an embrasure that is too wide, the balloon flattens out, assumes a blunted shape, and has a shallow sulcus. If the embrasure is ideal width, the papilla assumes a pointed form, has a sulcus of 2.5 to 3.0mm, and is healthy. If the embrasure is too narrow, the papilla may grow out to the facial and lingual, form a col, and become inflamed.
This suggestion can be applied when evaluating a papilla that does not adequately fill the interproximal embrasure. First, the dentist measures the distance from the papilla tip to the bone crest. If this distance is less than 5mm, the dentist can compress the balloon by adding restorative material to the mesial and distal tooth walls lateral to the papilla. This will push the balloon (papilla) coronally up to the 5-mm distance from the bone crest. If the distance from the bone to the papilla is 5mm or greater, the proximal contact must move apically to the top of the existing papilla (Fig. 5.51). When adjacent roots diverge, the proximal contact has moved coronally, and the interproximal embrasure is enlarged. Orthodontic movement to parallel the roots may improve the contact location, narrow the embrasure, and result in a taller, more pointed papilla (Fig. 5.52).
 Fig. 5.51 (A) Papilla does not fill embrasure. (B) Arrows indicate proposed subgingival extension of laminate veneer pushing papilla laterally. (C) Laminate veneers create long incisal contact. The definitive result is that the papilla has been forced into a smaller defined shape, which creates a taller, more pointed papilla.
Fig. 5.51 (A) Papilla does not fill embrasure. (B) Arrows indicate proposed subgingival extension of laminate veneer pushing papilla laterally. (C) Laminate veneers create long incisal contact. The definitive result is that the papilla has been forced into a smaller defined shape, which creates a taller, more pointed papilla.
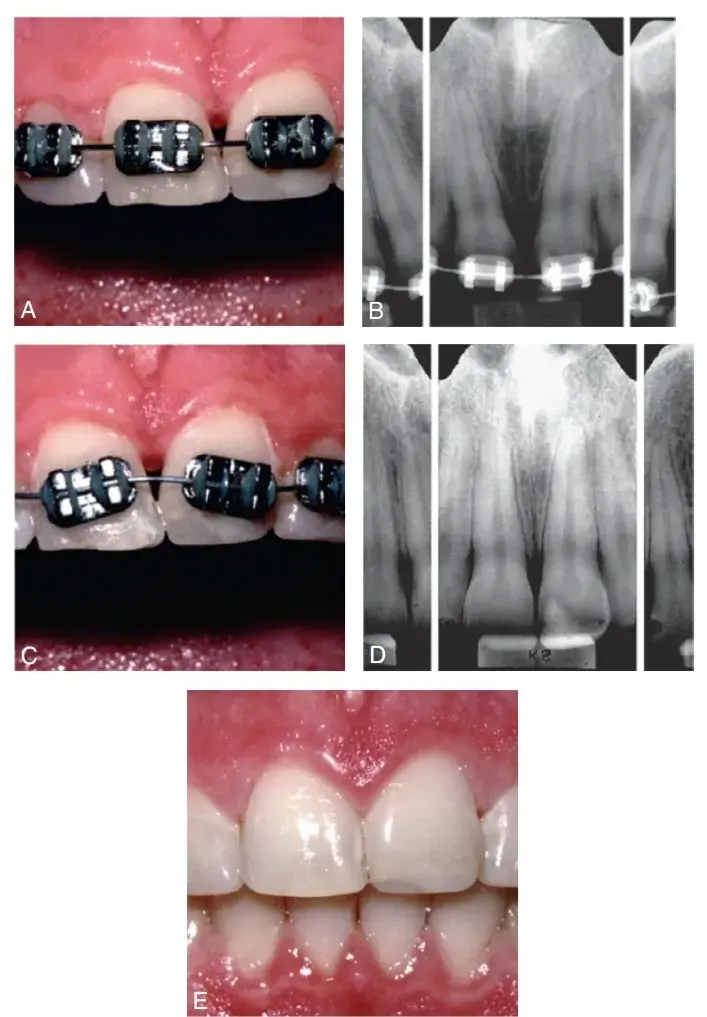 Fig. 5.52 (A) The papilla between teeth #8 and #9 does not fill the embrasure. (B) Radiograph reveals that the roots diverge, which results in a lack of pressure on the papilla. (C) Orthodontics used to reposition the roots. (D) Radiograph reveals that the roots are now correctly aligned. (E) The papilla now fills the entire embrasure. (From Newman MG, et al. Carranza's Clinical Periodontology. 10th ed. St. Louis: Saunders; 2006.)Double
Fig. 5.52 (A) The papilla between teeth #8 and #9 does not fill the embrasure. (B) Radiograph reveals that the roots diverge, which results in a lack of pressure on the papilla. (C) Orthodontics used to reposition the roots. (D) Radiograph reveals that the roots are now correctly aligned. (E) The papilla now fills the entire embrasure. (From Newman MG, et al. Carranza's Clinical Periodontology. 10th ed. St. Louis: Saunders; 2006.)Double
OVATE PONTICS
The extraction of a tooth entails removal of the proximal contact and half of the interproximal embrasure; as a consequence, the papilla is no longer compressed but flattens out, and esthetics are compromised. The papilla can be maintained if at the time of extraction an ovate pontic is created that will provide the proximal contact and lateral embrasure form needed to support the papilla. Ovate pontics are usually inserted 2.5mm into the extraction site. The size and shape of the ovate pontic should be comparable to the morphology of the extracted tooth. A site preservation bone grafting procedure should be performed at the time of the extraction. If bone levels remain stable, the papilla will also be stable.
A well-formed ovate pontic will seal the extraction socket and aid in retaining the bone graft within the socket. After 4 weeks, the ovate pontic should be reduced to extend into the socket 1.5mm to allow for oral hygiene (Fig. 5.53). Adequate edentulous ridges can be shaped to support ovate pontics. The receptor site is created with a diamond rotary instrument, an electrosurgery or radiosurgery unit, or a laser.
The receptor site is carved concave in the anterior aspect and slightly flatter in the posterior aspect. For esthetic reasons, its depth should be 1.0 to 1.5mm on the facial aspect to help create the appearance of a tooth emerging from a sulcus. The thickness of the gingival tissue between the bone and the newly created site for the ovate pontic must be at least 2mm, lest rebound of the gingiva will occur. If the thickness is less, bone must be removed.
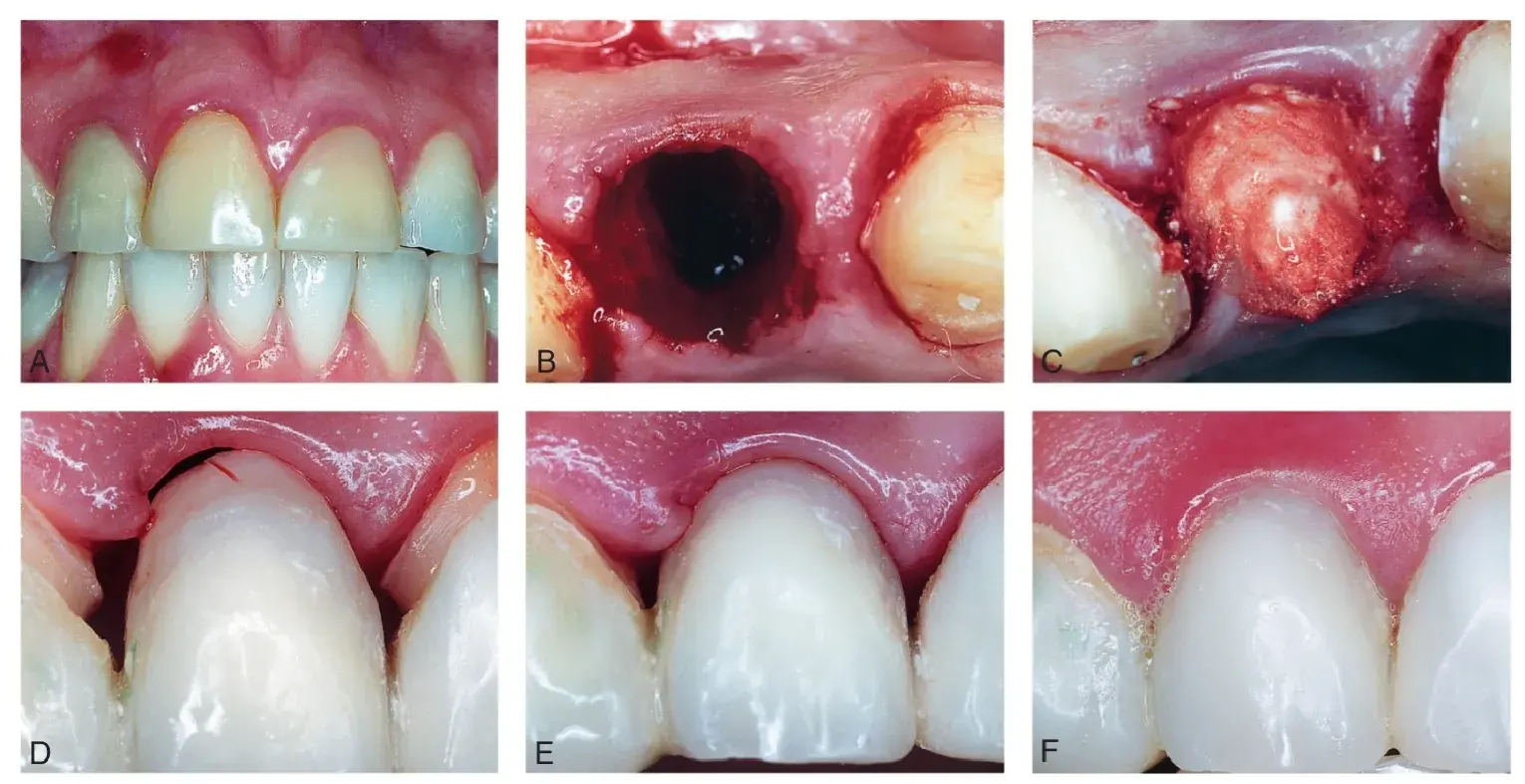 Fig. 5.53 (A) Maxillary right lateral incisor has failed despite endodontic treatment. (B) Socket after atraumatic tooth extraction. (C) Socket is filled with bone graft. (D) Interim fixed partial denture is fabricated. The ovate pontic extends 2.5mm into the socket and makes an excellent seal of the bone graft, as well as providing lateral support for the gingival papilla. (E) Healing of extraction site after 8 weeks. (F) Definitive restoration with a well-maintained papilla. (From Newman MG, et al. Carranza's Clinical Periodontology. 10th ed. St. Louis: Saunders; 2006.)
Fig. 5.53 (A) Maxillary right lateral incisor has failed despite endodontic treatment. (B) Socket after atraumatic tooth extraction. (C) Socket is filled with bone graft. (D) Interim fixed partial denture is fabricated. The ovate pontic extends 2.5mm into the socket and makes an excellent seal of the bone graft, as well as providing lateral support for the gingival papilla. (E) Healing of extraction site after 8 weeks. (F) Definitive restoration with a well-maintained papilla. (From Newman MG, et al. Carranza's Clinical Periodontology. 10th ed. St. Louis: Saunders; 2006.)
IMPLANT SITE MAINTENANCE AND DEVELOPMENT
Site development for dental implants in areas with insufficient bone consists of elevation of a gingival flap, placement of a bone graft, covering the bone graft with a barrier membrane, and releasing incisions so the flap can be elevated over the graft and membrane to allow tension free primary closure. Implant site development is highly technique sensitive (Fig. 5.54). The primary closure of the flap has to be maintained for 10 to 12 weeks to ensure maximum bone growth. The mobility of the gingival flap necessary to allow tension free closure results in gingival tissue that has been thinned with a compromised blood supply. The placement of a removable prosthesis to provide esthetics during the healing phase may inflict additional stress on this delicate area. Similarly, mastication over an unprotected gingival flap increases the risk for exposure of the membrane and bone graft. Short-term maintenance of teeth that have been deemed to have a poor or hopeless prognosis can allow them to serve as abutments for a fixed interim restoration that protects the gingival flap.
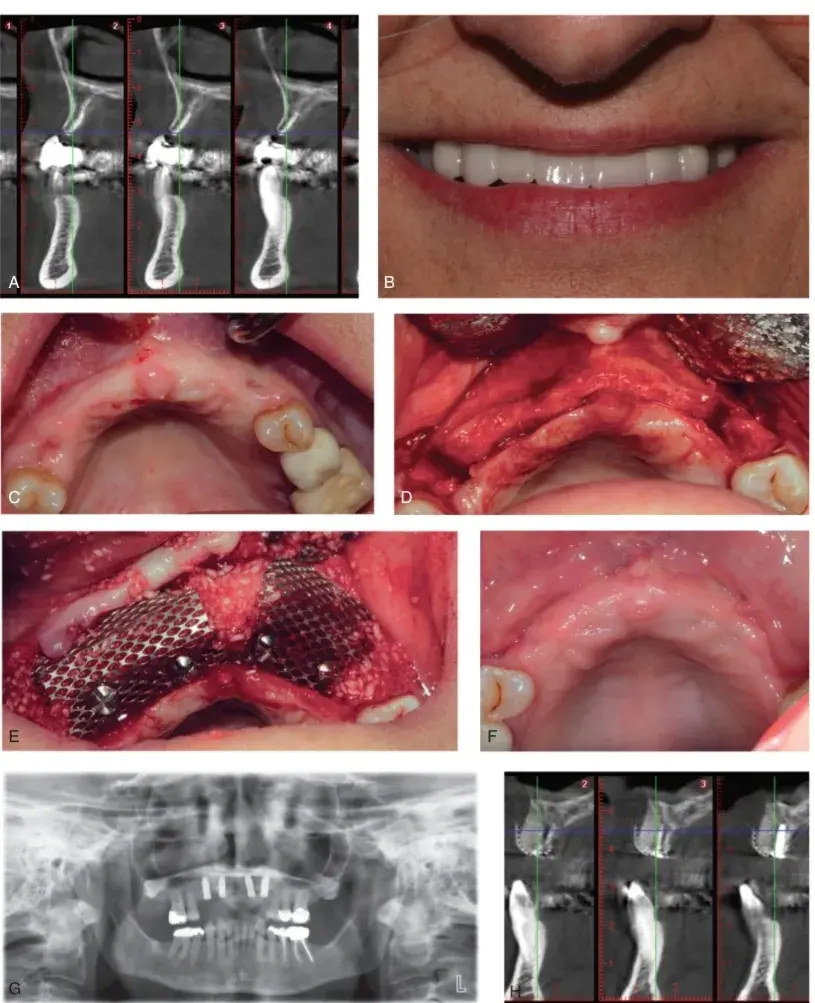 Fig. 5.54 (A) Radiographs of severely resorbed maxillary anterior ridge. (B and C) Pretreatment smile and edentulous ridge. (D) Initial full-thickness flap reflected. (E) Edentulous ridge has been decorticated, a bone graft has been placed, and two titanium membranes secured with screws provide space and stability. A resorbable membrane will be placed, and the flap will be sutured in layers. (F) Appearance 4 months after surgery. (G) Panoramic radiograph of four implants placed in the augmented ridge. (H) Radiograph of the significant bone growth in comparison with (A).
Fig. 5.54 (A) Radiographs of severely resorbed maxillary anterior ridge. (B and C) Pretreatment smile and edentulous ridge. (D) Initial full-thickness flap reflected. (E) Edentulous ridge has been decorticated, a bone graft has been placed, and two titanium membranes secured with screws provide space and stability. A resorbable membrane will be placed, and the flap will be sutured in layers. (F) Appearance 4 months after surgery. (G) Panoramic radiograph of four implants placed in the augmented ridge. (H) Radiograph of the significant bone growth in comparison with (A).
EXTRACTION SEQUELAE
After a routine extraction, the average bone and gingival loss for a maxillary anterior tooth is 2.0 to 3.5mm of vertical bone and gingival tissue, along with 1 to 2mm of buccal and lingual bone and gingival loss. This loss will cause alterations in gingival margin levels between the prosthetic replacement tooth and the adjacent teeth. Patients with a thin biotype will develop more recession and bone loss. A thick biotype will have less bone and gingival loss. Various bone grafts alone or in combination with barrier membranes have been employed at the time of extraction to prevent bone and gingival loss; collectively, these techniques are referred to as site preservation. These regenerative measures are partially successful and can minimize bone and gingival loss.
In the best-case scenario, a patient with a thick biotype will lose only 1 to 2mm of vertical bone and gingiva after site preservation techniques in maxillary anterior teeth. A patient with a thin biotype may lose a severe amount of bone and gingiva (5 to 7mm) after an atraumatic extraction of a maxillary anterior tooth, in spite of a site preservation procedure. The facial bone thickness is less than 1mm in thin biotypes, and the compromised blood supply cannot maintain bone vitality during the healing process. In the most challenging scenario, a patient with a thin biotype and a high smile line, displaying 2 to 4mm of gingiva, is in need of a maxillary anterior extraction. No amount of site preservation or regenerative therapy after an extraction will prevent significant loss of bone and gingiva, which will likely result in an esthetic failure. In such cases orthodontic extrusion can be a useful adjunct to minimize post-extraction gingival and bony changes.
ORTHODONTIC EXTRUSION
In esthetic areas, orthodontic extrusion can minimize the risk for significant gingival changes following an extraction or correction of a BWV.87–89 A slow (0.5 to 2mm per month), low-force extrusion (15 to 50g) will bring new alveolar bone and gingiva with the tooth as it moves coronally (see Chapter 6). The tooth is extruded several millimeters beyond the adjacent teeth and stabilized for 2 months. The resulting excess gingiva and excess bone allow these tissues to approximate normal levels after extraction. An alternative approach is rapid orthodontic extrusion, in which a root is quickly moved out of the alveolus over a matter of weeks. Strong orthodontic forces are used, and a supracrestal fiberotomy (an intrasulcular incision to separate the periodontal ligament from the root surface) is performed every week to prevent the bone and gingiva from emerging with the extruding tooth. The tooth is then stabilized for 3 months, and bone and gingiva are evaluated before the definitive restoration is provided. Orthodontic extrusion can also be utilized to develop bone or expose more tooth structure for fixed prosthodontics. Whether rapidly or over a long period of time, when teeth are orthodontically erupted it is important to carefully monitor the occlusion and adjust the erupting teeth so that they have space to move and are not traumatized from occlusal forces.
Rapid orthodontic extrusion without supracrestal fiberotomy can be utilized to force eruption of the “hopeless” tooth 3mm or more. This will move the gingiva and bone along with the tooth more coronally and loosen the periodontal ligament. As a result, the tooth will be easier to extract, 2 to 4mm of excessive tissue and bone will undergo normally representative post extraction loss, and gingival levels will match those of the adjacent tooth. This concept of orthodontic extrusion can be taken a step further and used for implant site development in areas lacking sufficient bone, especially in a vertical direction (Fig. 5.55). Amato et al87 utilized orthodontic extrusion to extrude 32 teeth with hopeless prognoses (mean: 6.2mm). They were able to gain 4.0mm of vertical bone height and 3.9mm of vertical gingival movement. Together, with the increase in vertical gingival height, a coronal papilla movement also resulted. Light continuous pressure extrudes teeth 1 to 2mm per month. To finalize the orthodontic extrusion, the tissues should be stabilized for 2 to 3 months before extraction, to allow the newly formed bone time to mature and mineralize.
Orthodontic movement of “hopeless” teeth for implant site development should be considered as equally efficacious as surgical implant site development. Augmentation of edentulous ridge width by approximately 3mm is surgically predictable with particulate bone grafts and barrier membranes.
Augmentation of edentulous ridge height is less feasible. The standard treatment is use of a vital block of autogenous bone. Sources of autogenous bone block grafts include the ascending ramus, the chin, the hip, and the femur. Additional tissue to cover large block grafts is often harvested from the leg before the block graft itself. Orthodontics is more predictable and less invasive. Lateral augmentation of the newly developed vertical bone height from orthodontics is made more straightforward with the additional thick, keratinized gingival tissue.
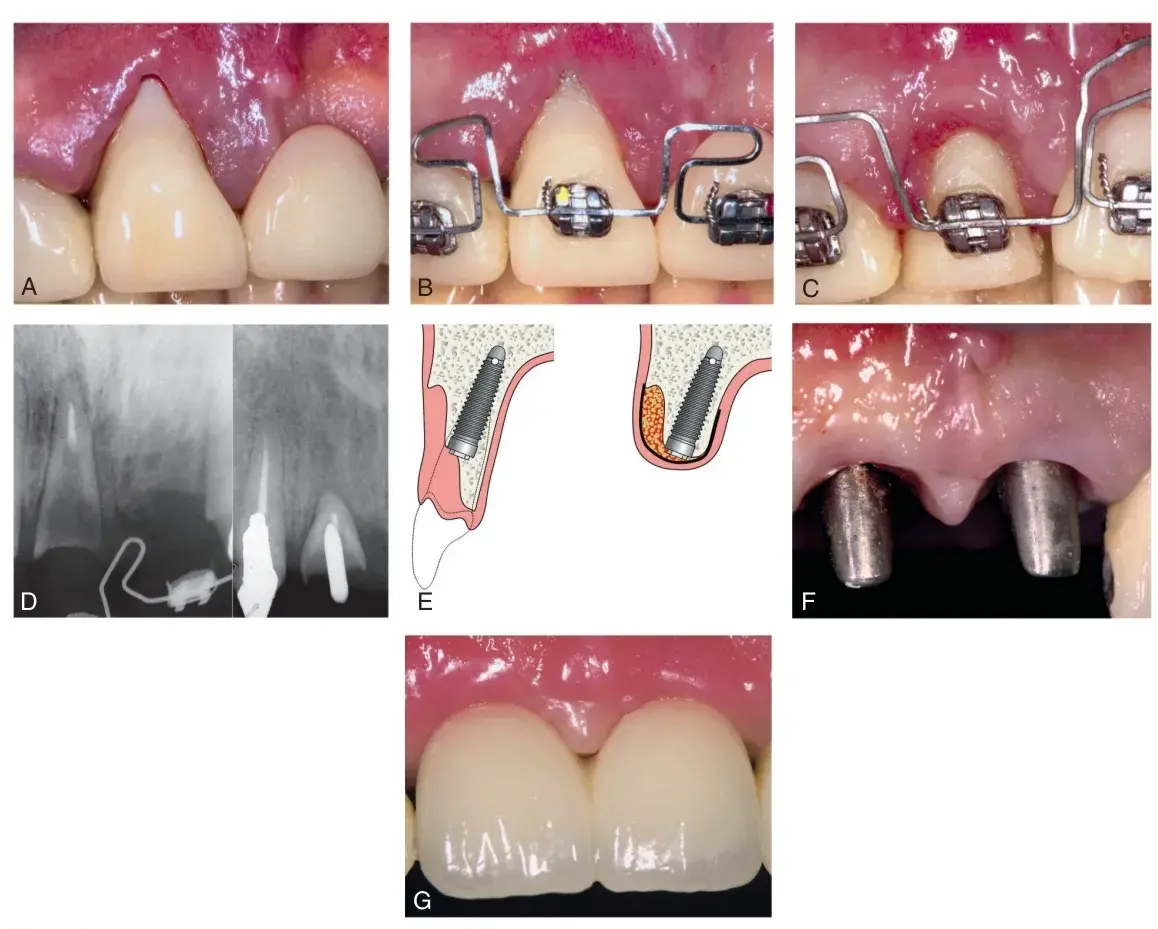 Fig. 5.55 (A) Failing maxillary right central incisor in a patient with a thin biotype and gingival recession. Extraction would create a severe esthetic challenge. (B) Orthodontic forced eruption (OFE) is initiated to move the tooth incisally and palatally. (C) Note the improved gingival contour. (D) Radiographs demonstrating almost 10mm of OFE. (E) Illustration of bone development incisally and in width, achieved with OFE. (F) Implants placed immediately in conjunction with lateral ridge augmentation. (G) Final esthetic results that would have been very difficult to achieve without the aid of OFE. (From Watanabe T, et al. Creating labial bone for immediate implant placement: a minimally invasive approach by using orthodontic therapy in the esthetic zone. J Prosthet Dent. 2013;110:435.)
Fig. 5.55 (A) Failing maxillary right central incisor in a patient with a thin biotype and gingival recession. Extraction would create a severe esthetic challenge. (B) Orthodontic forced eruption (OFE) is initiated to move the tooth incisally and palatally. (C) Note the improved gingival contour. (D) Radiographs demonstrating almost 10mm of OFE. (E) Illustration of bone development incisally and in width, achieved with OFE. (F) Implants placed immediately in conjunction with lateral ridge augmentation. (G) Final esthetic results that would have been very difficult to achieve without the aid of OFE. (From Watanabe T, et al. Creating labial bone for immediate implant placement: a minimally invasive approach by using orthodontic therapy in the esthetic zone. J Prosthet Dent. 2013;110:435.)
SUMMARY
The periodontium that supports fixed prosthodontics is a conduit to immediate and long-term success. Preprosthetic procedures consist of periodontal supportive therapy (oral hygiene instructions, prescription rinses, and professional cleanings), surgically and orthodontically repositioning bone and free gingival margins. If a clinician were to overlook the periodontium in the initial phases of fixed prosthodontic care, complications will quickly develop before completion or immediately after therapy. Unesthetic positions of crown margins and pontics could result, as well with early dental implant failure. Maintenance is the most important factor for long-term success. Research makes it very clear that without maintenance, fixed prosthodontics will succumb to early failure.
There are additional details about complex perio-restorative cases treatment that you can obtain in course Advanced periodontology: surgical protocols by Dr. Daniel Melker.
STUDY QUESTIONS
Discuss and compare the 10 years’ success of surgical pocket reduction surgery versus scaling and root planning.
Two- to three-month supportive periodontal maintenance (SPT) is effective in reducing the recurrence of periodontal disease in most patients. What other benefits occur as a result of frequent SPT?
Teeth with a questionable periodontal prognosis can often be maintained for a considerable time period. Please discuss how this affects the restorative treatment options.
Discuss the effect of thick or thin gingival biotype on the amount of anticipated gingival recession after an anterior extraction.
Describe the effect on crown-to-root ratio of surgical crown lengthening versus orthodontic forced eruption.
At the time of extraction of a maxillary central incisor, is a socket preservation bone graft sufficient to preserve the gingival papilla?
Biologic shaping (BS) minimizes changes to the crown to root ratio. Please discuss the reason for the minimal changes to the crown to root ratio.
A mandibular first molar with a buccal class 1 furcation has received BS and the roof of the furcation was eliminated.
How should the future crown be modified?
The buccal flap reflection for BS is a split-thickness flap.
What are the advantages of a split thickness flap.
What is the difference between osteotomy and osteoplasty?
References
Lindhe J, et al. Clinical Periodontology and Implant Dentistry; vol
5th ed. Oxford, U.K: Wiley-Blackwell; 2008.
Newman MG, ed. Carranza's Clinical Periodontology. 11th ed. St. Louis: Elsevier/Saunders; 2012.
Hirschfeld L, Wasserman B. A long-term survey of tooth loss in 600 treated periodontal patients. J Periodontol. 1978;49:225.
Bostanci HS, Arpak MN. Long-term evaluation of surgical periodontal treatment with and without maintenance care. J Nihon Univ Sch Dent. 1991;33:152.
Svärdström G, Wennström JL. Periodontal treatment decisions for molars: an analysis of influencing factors and long-term outcome. J Periodontol. 2000;71:579.
McFall Jr WT. Tooth loss in 100 treated patients with periodontal disease. A long-term study. J Periodontol. 1982;53:539.
Wood WR, et al. Tooth loss in patients with moderate periodontitis after treatment and long-term maintenance care. J Periodontol. 1989;60:516.
Eke PI, et al. Prevalence of periodontitis in adults in the United States: 2009 and 2010. J Dent Res. 2012;91:914.
Kim JK, et al. Prevalence of oral health problems in U.S. adults, NHANES 1999-2004: exploring differences by age, education, and race/ethnicity. Spec Care Dent. 2012;32:234.
Dye BA, et al. Trends in oral health status: United States, 1988–1994 and 1999–2004. Vital Health Stat. 2007;11:1.
Slots J. Low-cost periodontal therapy. Periodontol. 2012;60:110 2000.
Drisko CH. Nonsurgical periodontal therapy. Periodontol. 2001;25:77.
Reddy MS, et al. Periodontal disease progression. J Periodontol. 2000;71:1583.
Kinney JS, et al. Oral fluid-based biomarkers of alveolar bone loss in periodontitis. Ann N Y Acad Sci. 2007;1098:230.
Belstrøm D, et al. Differences in bacterial saliva profile between periodontitis patients and a control cohort. J Clin Periodontol. 2014;41:104.
Weinberg MA, Hassan H. Bleeding on probing: what does it mean? Gen Dent. 2012;60:271.
Goodson JM. Diagnosis of periodontitis by physical measurement: interpretation from episodic disease hypothesis. J Periodontol. 1992;63:373.
Listgarten MA. Periodontal probing: what does it mean? J Clin Periodontol. 1980;7:165.
Heitz-Mayfield LJA, Lang NP. Surgical and nonsurgical periodontal therapy. Learned and unlearned concepts. Periodontol. 2013;62:218 2000.
Sanz I, et al. Nonsurgical treatment of periodontitis. J Evid Based Dent Pract. 2012;12:76–86.
Hallmon WW, Rees TD. Local anti-infective therapy: mechanical and physical approaches. A systematic review. Ann Periodontol. 2003;8:99.
McLeod DE. A practical approach to the diagnosis and treatment of periodontal disease. J Am Dent Assoc. 2000;131:483.
Hempton TJ, Dominici JT. Contemporary crown-lengthening therapy: a review. J Am Dent Assoc. 2010;141:647.
Nyman S, et al. Periodontal surgery in plaque-infected dentitions. J Clin Periodontol. 1977;4:240.
Rylander H. Changing concepts of periodontal treatment: surgical and non-surgical. Int Dent J. 1988;38:163.
Pihlstrom BL, et al. Comparison of surgical and nonsurgical treatment of periodontal disease. A review of current studies and additional results after years. J Clin Periodontol. 1983;10:524.
Dentino A, et al. Principles of periodontology. Periodontol. 2013;61:16 2000.
Lang NP, et al. Absence of bleeding on probing. An indicator of periodontal stability. J Clin Periodontol. 1990;17:714.
Lang NP, et al. Bleeding on probing. A predictor for the progression of periodontal disease? J Clin Periodontol. 1986;13:590.
Axelsson P, et al. The effect of various plaque control measures on gingivitis and caries in schoolchildren. Community Dent Oral Epidemiol. 1976;4:232.
Axelsson P, Lindhe J. Effect of oral hygiene instruction and professional toothcleaning on caries and gingivitis in schoolchildren. Community Dent Oral Epidemiol. 1981;9:251.
Chambrone L, Chambrone L. Results of a 20-year oral hygiene and prevention programme on caries and periodontal disease in children attended at a private periodontal practice. Int J Dent Hyg. 2011;9:155.
Axelsson P, et al. On the prevention of caries and periodontal disease. J Clin Periodontol. 1991;18:182.
Persson GR. Perspectives on periodontal risk factors. J Int Acad Periodontol. 2008;10:71.
Page RC, Beck JD. Risk assessment for periodontal diseases. Int Dent J. 1997;47:61.
Garcia RI, et al. Risk calculation and periodontal outcomes. Periodontol. 2009;50:65.
Halperin-Sternfeld M, Levin L. Do we really know how to evaluate tooth prognosis? A systematic review and suggested approach. Quintessence Int. 2013;44:447.
Aimetti M. Nonsurgical periodontal treatment. Int J Esthet Dent. 2014;9:251.
Segelnick SL, Weinberg MA. Reevaluation of initial therapy: when is the appropriate time? J Periodontol. 2006;77:1598.
Claffey N, Egelberg J. Clinical indicators of probing attachment loss following initial periodontal treatment in advanced periodontitis patients. J Clin Periodontol. 1995;22:690.
Wojcik MS, et al. Retained “hopeless” teeth: lack of effect periodontally-treated teeth have on the proximal periodontium of adjacent teeth 8-years later. J Periodontol. 1992;63:663.
Chronopoulos V, et al. Tooth- and tissue-supported provisional restorations for the treatment of patients with extended edentulous spans. J Esthet Restor Dent. 2009;21:7.
Cortes A, et al. Transition from failing dentition to full-arch fixed implant-supported prosthesis with a staged approach using removable partial dentures: a case series. J Prosthodont. 2014;23:328.
Rokn AR, et al. Implant site development by orthodontic forced eruption of nontreatable teeth: a case report. Open Dent J. 2012;6:99.
Horowitz F, et al. A review on alveolar ridge preservation following tooth extraction. J Evid Based Dent Pract. 2012;1:149.
Bouri A, et al. Width of keratinized gingiva and the health status of supporting tissue around dental implants. Int J Oral Maxillofac Implant. 2008;23:323.
Warrer K, et al. Plaque-induced peri-omplantitis in the presence or absence of keratinized mucosa. An experimental study in monkeys. Clin Oral Implant Res. 1995;6:131.
Schmidt JC, et al. Biologic width dimensions—a systematic review. J Clin Periodontol. 2013;40:493.
Smith RG, et al. Variations in the clinical sulcus depth of healthy human gingiva: a longitudinal study. J Periodont Res. 1996;31:181.
Valderhaug J, Heloe LA. Oral hygiene in a group of supervised patients with fixed prostheses. J Periodontol. 1977;48:221.
Moretti LAC, et al. The influence of restorations and prosthetic crowns finishing lines on inflammatory levels after non-surgical periodontal therapy. J Int Acad Periodontol. 2011;13:65.
Drisko CL. Periodontal self-care: evidence-based support. Periodontol. 2013;62:243 2000.
Schätzle M, et al. The influence of margins of restorations on the periodontal tissues over 26 years. J Clin Periodontol. 2001;28:57.
Reeves WG. Restorative margin placement and periodontal health. J Prosthet Dent. 1991;66:733.
Felton DA, et al. Effect of in vivo crown margin discrepancies on periodontal health. J Prosthet Dent. 1991;65:357.
Kosyfaki P, et al. Relationship between crowns and the periodontium: a literature update. Quintessence Int. 2010;41:109.
Maynard Jr JG, Wilson RD. Physiologic dimensions of the periodontium significant to the restorative dentist. J Periodontol. 1979;50:170.
Nugala B, et al. Biologic width and its importance in periodontal and restorative dentistry. J Conserv Dent. 2012;15:12.
Sanavi F, et al. Biologic width and its relation to periodontal biotypes. J Esthet Dent. 1998;10:157.
Cook DR, et al. Relationship between clinical periodontal biotype and labial plate thickness: an in vivo study. Int J Periodontics Restor Dent. 2011;31:345.
Lee A, et al. Soft tissue biotype affects implant success. Implant Dent. 2011;20:e38.
De Rouck T, et al. The gingival biotype revisited: transparency of the periodontal probe through the gingival margin as a method to discriminate thin from thick gingiva. J Clin Periodontol. 2009;36:428.
Sharma A, et al. Short clinical crowns (SCC)—treatment considerations and techniques. J Clin Exp Dent. 2012;4:e230.
Braga G, Bocchieri A. A new flapless technique for crown lengthening after orthodontic extrusion. Int J Periodontics Restor Dent. 2012;32:81.
McGuire MK, Scheyer ET. Laser-assisted flapless crown lengthening: a case series. Int J Periodontics Restor Dent. 2011;31:357.
Tucker L, et al. Combining perio-restorative protocols to maximize function. Gen Dent. 2012;60:280.
Melker D, Richardson C. Root reshaping: an integral component of periodontal surgery. Int J Periodontics Restor Dent. 2001;21:296.
Strupp W, Melker DJ. Maximizing aesthetics using a combined periodontal- restorative protocol. Dent Today. 2003;22:60.
Melker D. Biologic shaping. J Impl Adv Clin Dent. 2009;1:13.
Satheesh K, et al. The CEJ: a biofilm and calculus trap. Compend Contin Educ Dent. 2011;32:30.
Bugueno I, et al. Porphyromonas gingivalis bypasses epithelial barrier and modulates fibroblastic inflammatory response in an in vitro 3D spheroid model. Sci Rep. 2018;8:14914.
Tarnow DP, et al. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992;63:995–996.
Newman MG, et al. eds. Carranza’s Clinical Periodontology. 10th ed. St. Louis, Mo: Elsevier/Saunders; 2006:1059.
Zitzmann NU, et al. The ovate pontic design: a histologic observation in humans. J Prosthet Dent. 2002;88:375.
Jensen SS, Terheyden H. Bone augmentation procedures in localized defects in the alveolar ridge: clinical results with different bone grafts and bone-substitute materials. Int J Oral Maxillofac Implant. 2009;24:218.
Chiapasco M, et al. Bone augmentation procedures in implant dentistry. Int J Oral Maxillofac Implant. 2009;24:237.
Thalmair T, et al. Dimensional alterations of extraction sites after different alveolar ridge preservation techniques—a volumetric study. J Clin Periodontol. 2013;40:721.
Wang RE, Lang NP. Ridge preservation after tooth extraction. Clin Oral Implants Res. 2012;23:147.
Chen ST, Buser D. Clinical and esthetic outcomes of implants placed in postextraction sites. Int J Oral Maxillofac Implant. 2009;24:186.
Cardaropoli D, et al. Relationship between the buccal bone plate thickness and the healing of postextraction sockets with/without ridge preservation. Int J Periodontics Restor Dent. 2014;34:211.
Malchiodi L, et al. Evaluation of the esthetic results of nonfunctional immediately loaded postextraction implants in the maxilla: correlation between interproximal alveolar crest and soft tissues at 3 years of follow-up: esthetic evaluation of immediately loaded postextraction implants. Clin Implant Dent Relat Res. 2013;15:130.
Den Hartog L, et al. Treatment outcome of immediate, early and conventional single-tooth implants in the aesthetic zone: a systematic review to survival, bone level, soft-tissue, aesthetics and patient satisfaction. J Clin Periodontol. 2008;35:1073.
Ferrus J, et al. Factors influencing ridge alterations following immediate implant placement into extraction sockets. Clin Oral Implant Res. 2010;21:22.
Chappuis V, et al. Ridge alterations post-extraction in the esthetic zone: a 3D analysis with CBCT. J Dent Res. 2013;92:195S.
Eliasova P, et al. Implant site development in the distal region of the mandible: bone formation and its stability over time. Am J Orthod Dentofac Orthop. 2014;145:333.
Zakhary IE, et al. Alveolar ridge augmentation for implant fixation: status review. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114:S179.
Amato F, et al. Implant site development by orthodontic forced extraction: a preliminary study. Int J Oral Maxillofac Implant. 2012;27:411.
Kozlovsky A, et al. Forced eruption combined with gingival fiberotomy. A technique for clinical crown lengthening. J Clin Periodontol. 1988;15:534.
Barros L, et al. Six-year follow-up of maxillary anterior rehabilitation with forced orthodontic extrusion: achieving esthetic excellence with a multidisclipinary approach. Am J Orthod Dentofac Orthop. 2013;144:607.
Urban IA, et al. Vertical ridge augmentation using guided bone regeneration (GBR) in three clinical scenarios prior to implant placement: a retrospective study of 35 patients 12 to 72 months after loading. Int J Oral Maxillofac Implant. 2009;24:502.
Al-Mubarek S, et al. Comparative evaluation of adjunctive oral irrigation in diabetics. J Clin Periodontol. 2002;29:295.
Barnes CM, et al. Comparison of irrigation to floss as an adjunct to tooth brushing: effect on bleeding, gingivitis, and supragingival plaque. J Clin Dent. 2005;16:71.
Brownstein CN, et al. Irrigation with chlorhexidine to resolve naturally occurring gingivitis: a methodologic study. J Clin Periodontol. 1990;17:588.
Burch JG, et al. A two-month study of the effects of oral irrigation and automatic toothbrush use in an adult orthodontic population with fixed appliances. Am J Orthod Dentofac Orthop. 1994;106:121.
Chaves ES, et al. Mechanism of irrigation effects on gingivitis. J Periodontol. 1994;65:1016.
Ciancio SG, et al. Effect of a chemotherapeutic agent delivered by an oral irrigation device on plaque, gingivitis, and subgingival microflora. J Periodontol. 1989;60:310.
Cutler CW, et al. Clinical benefits of oral irrigation for periodontitis are related to reduction of pro-inflammatory cytokine levels and plaque. J Clin Periodontol. 2000;27:134.
Felo A, et al. Effects of subgingival chlorhexidine irrigation on perio-implant maintenance. Am J Dent. 1997;10:107.
Fine JB, et al. Short-term microbiological and clinical effects of subgingival irrigation with an antimicrobial mouthrinse. J Periodontol. 1994;65:30.
Flemmig TF, et al. Adjunctive supragingival irrigation with acetylsalicylic acid in periodontal supportive therapy. J Clin Periodontol. 1995;22:427.
Flemmig TF, et al. Supragingival irrigation with 0.06% chlorhexidine in naturally occurring gingivitis I. 6 month clinical observations. J Periodontol. 1990;61:112.
Jolkovsky DL, et al. Clinical and microbiological effects of subgingival and gingival marginal irrigation with chlorhexidine gluconate. J Periodontol. 1990;61:663.
Lobene RR. The effect of a pulsed water pressure-cleansing device on oral health. J Periodontol. 1969;40:51.
Newman MG, et al. Effectiveness of adjunctive irrigation in early periodontitis: multi-center evaluation. J Periodontol. 1994;65:224.
Sharma NC, et al. Effect of a dental water jet with orthodontic tip on plaque and bleeding in adolescent patients with fixed orthodontic appliances. Am J Orthod Dentofacial Orthop. 2008;133:565.
Walsh TF, et al. Clinical effects of pulsed oral irrigation with 0.0% chlorhexidine digluconate in patients with adult periodontitis. J Clin Periodontol. 1992;19:245