Polyetheretherketone in Implant Prosthodontics: A Scoping Review
ABSTRACT
Purpose: To undertake a scoping review of the available research on the application of polyetheretherketone (PEEK) in implant prosthodontics, map the available literature in order to highlight possible gaps in knowledge and, if possible, extract clinical guidelines.
Materials and Methods: The literature on PEEK in implant prosthodontics published through August 2018 was identified with an online search of MEDLINE (via PubMed), Science Direct, Embase (via Ovid), and Google Scholar databases. Qualitative and quantitative syntheses were carried out for original research studies.
Results: The amount of published original research studies was found to be limited. PEEK was found to be applied as a material in the fabrication of implant-supported fixed dental prosthesis (IFDP) frameworks (43%), prosthetic implant abutments (35%), implant abutment screws (15%), and retention clips on implant bars (7%). Only 38% of the studies were clinical studies, while 15% were observational and 47% were in vitro. The studies identified did not permit the estimation of long-term survival nor success rates for any of the prosthetic components. The results only allowed a preliminary short-term assessment of PEEK IFDP frameworks, which presented satisfactory survival but alarming success rates over the first year of service.
Conclusion: In light of the paucity of evidence on the viability of PEEK as an implant-prosthodontic material, its use cannot yet be endorsed. Clinicians should heed the suggested protocols to improve mechanical performance and lower the incidence of prosthetic complications. Further high-quality research is needed for an enhanced understanding of the material’s viability.
Further details about implant-supported prosthetics are accessible for you to learn on our website.
INTRODUCING
Plastic materials have a broad range of applications today, and there are many different categories of polymers available. High-performance polymers are plastics that meet stringent requirements for temperature stability, chemical resistance, and mechanical properties. Since their formulations can be altered as required, these materials can be designed favoring any one of these characteristics over the others to meet specific objectives. High-performance polymers find many applications in many different fields, such as engineering, industry, and medicine (ie, medical devices).1,2
Polyetheretherketone (PEEK) is a polycyclic aromatic semi-crystalline thermoplastic polymer with mechanical properties that are favorable for biomedical applications. By incorporating hydroxyapatite particulates into a PEEK matrix, some authors have obtained a composite polymer that showed a tensile strength ranging from 49.0 to 83.3 MPa, which matches the lower limits of cortical bone (50 to 150 MPa).3 Thanks to its elastic behavior, which is similar to human bone, PEEK is widely used in spinal surgery, orthopedic surgery, and maxillofacial surgery as a bone and cartilage substitute.4,5
PEEK was first introduced in three forms of unfilled versions: PEEK-LT1, PEEK-LT2, and PEEK-LT3. Subsequently, fillers such as ceramics, hydroxyapatite, beta-calcium phosphate, and carbon fibers were added to the PEEK formula to increase its bioactivity and improve its mechanical properties, leading to materials such as BioHPP (Bredent).6,7 Many filled PEEK versions are now being used to manufacture biomedical implants.7 Due to its favorable mechanical properties, PEEK has also reached the field of dentistry, where it has been implemented in several areas. Combining its properties with the ongoing diffusion of CAD/CAM technology, PEEK components can now be digitally designed and then 3D printed, achieving high precision to meet clinical requirements.
A variety of reviews have discussed the applications of PEEK in oral implantology and tooth-supported prosthodontics, which include components for tooth-supported fixed dental prostheses (FDPs), tooth-supported removable dental prostheses (RDPs), bioactive nanocomposites, and dental implants.8–15
PEEK was initially introduced to the implant prosthodontics field as a material for the fabrication of interim restoration components such as implant abutments, thanks to its fabrication feasibility with CAD/CAM, its affordable price, and its better mechanical performance compared to common resin materials.16 However, no review articles focusing exclusively on PEEK’s role in implant prosthodontics have been identified. It has been reported by several authors that the evidence regarding PEEK in dentistry is still limited in quantity2,13; thus, a scoping review seems to be the most appropriate type of review article to conduct on this topic in order to assess whether conducting a further systematic review on the application of this polymer in implant prosthodontics would be indicated. Therefore, the present scoping review was conducted in order to systematically map the research done in this area, as well as to identify any existing gaps in knowledge regarding PEEK material behavior when applied as an implant-prosthodontic component. The following research question was formulated: What is known from the literature about the application of PEEK in implant prosthodontics?
MATERIALS AND METHODS
A search of the literature was carried out in the following databases: MEDLINE via PubMed, Science Direct, and Google Scholar. [AU: And Embase via Ovid, as mentioned in the Abstract?] The following keyword search strategy was applied: PEEK OR polyetheretherketone OR poly-ether-ether-ketone OR high-performance polymer* OR high performance polymer* OR BioHPP AND (dentistry OR implant-prosthodontics). As a search filter, only articles published through August 31, 2018, were considered. Additionally, reference lists and previous review articles were also screened for relevant articles. Regarding the Google Scholar database, only the first 300 results were considered, as suggested by Haddaway et al.17 No review protocol has been registered for this work.
The PRISMA Extension for Scoping Reviews (PRISMA-ScR) checklist was followed as a guideline for the correct reporting of the items required for this type of review.18
An initial assessment of article eligibility was performed by screening titles and abstracts, followed by a full-text analysis. The titles and abstracts of the search results were initially screened by two reviewers (A.P. and G.P.) for possible inclusion. To avoid excluding potentially relevant articles, abstracts providing an unclear result were included in the full-text analysis. The full texts of all possibly relevant studies were obtained for independent assessment by the two reviewers against the stated inclusion criteria. Disagreements were brought to an independent reviewer (M.G.) and resolved through discussion.
To be included in the preliminary evaluation, the following criteria had to be met by the article: abstract present; related to PEEK in its unfilled and filled presentations; and related to dentistry. To be included in the qualitative and quantitative syntheses, the following criteria had to be met: articles discussing PEEK’s applications in implant prosthodontics that registered variables linked to the relevant prosthetic component.
No discriminations were made regarding the manufacturing process of the material, its composition, its surface modification, or its veneering procedures. Only original research papers and case reports were considered for the qualitative and quantitative analyses. Historical and systematic reviews, book chapters, and letters to the editor were excluded from the analyses; however, if considered pertinent, they were used for contextualizing the material’s background.
One independent author [AU: Please provide their initials here] carried out the data charting, with the objective of extracting information regarding sample size, follow-up period, survival rate, success rate, fracture strength of the restoration, fracture strength of the prosthetic component, and complications. Descriptive statistical analysis was performed for the data that were deemed suitable. For human and animal studies that reported the necessary information, weighted arithmetic means for survival and success rates were calculated. Survival was considered as the presence of the prosthetic component inside the mouth at the time of observation. Success was considered as absence of complications at the time of observation.19 In case survival and success rates regarding the same application of the material were available from multiple studies, human and animal data were pooled separately. Interexaminer agreement was calculated using κ statistics.
RESULTS
A total of 1,910 articles were identified from the three databases searched (MEDLINE, Science Direct, and Google Scholar) (Fig 1). [AU: Not Embase?] After checking for duplicates, the titles and abstracts of 1,522 articles were screened. Of these articles, 146 were selected for a full-text assessment; of those, 13 were included in the qualitative and quantitative summaries after a full-text review (Table 1).6,7,20–30 During screening of the abstracts, a κ value of 0.91 for interexaminer agreement was calculated, and during full-text analysis, a κ value of 0.83 was observed. Disagreements were resolved through discussion between the reviewers. Different study designs were identified. In vivo clinical studies consisted of 38% (5 studies) of the total, but only 2 had a controlled design, and only 1 was randomized. In vivo observational studies consisted of 15% (2 studies) of the total, while in vitro research consisted of 47% (6 studies) of the total.
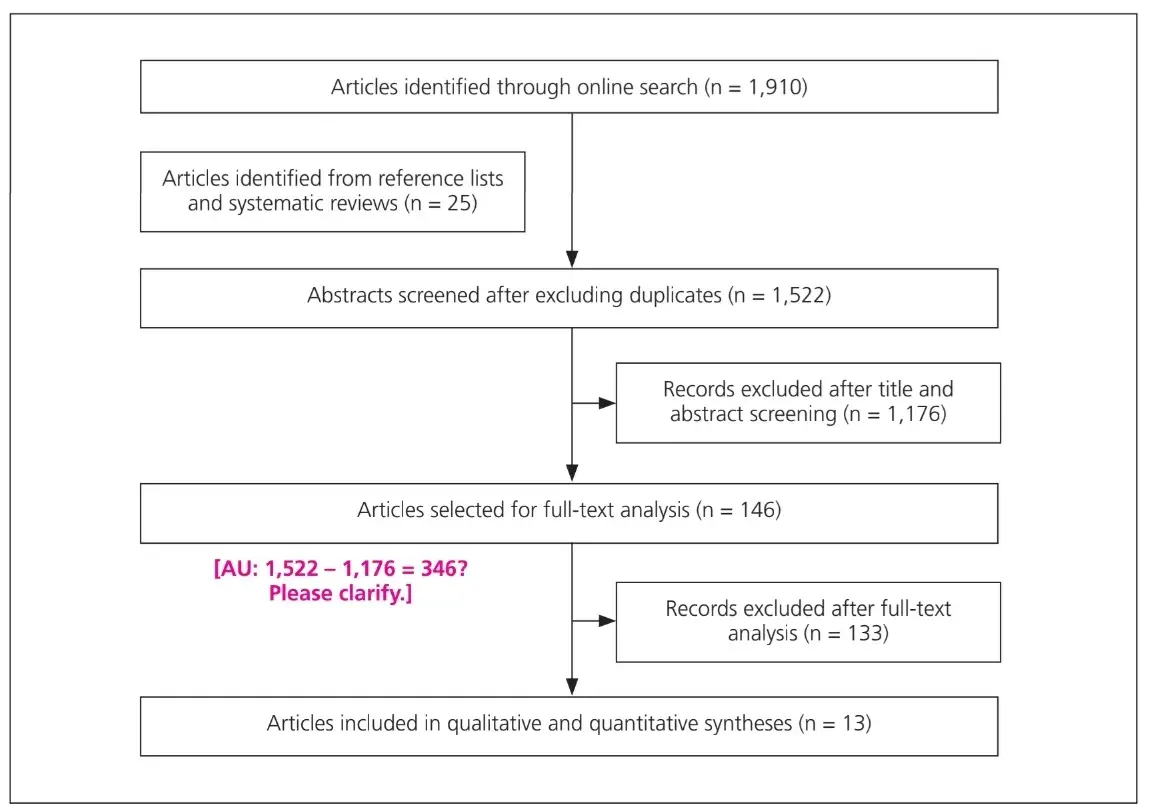 Fig 1 Flowchart of literature search protocol.
Fig 1 Flowchart of literature search protocol.
Table 1 Studies Included in Qualitative and Quantitative Syntheses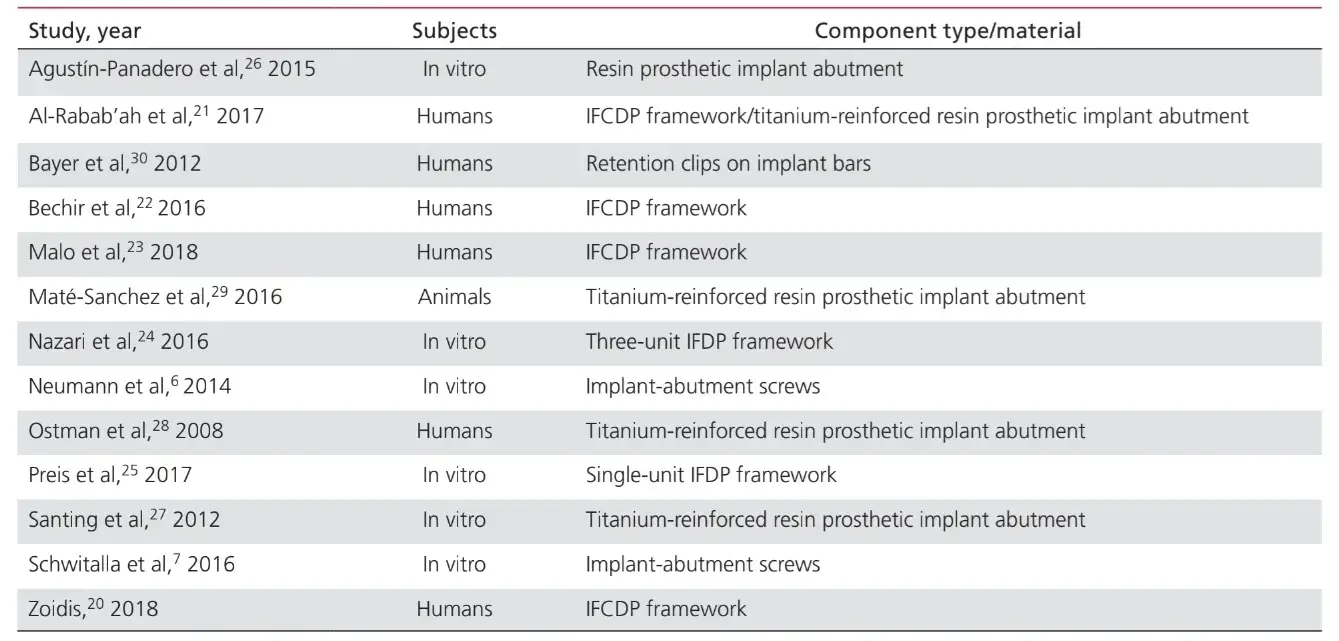
The applications for PEEK as a material for the manufacture of components involved in implant-prosthodontic rehabilitation procedures were: IFDP frameworks (43%); prosthetic implant abutments (35%); implant-abutment screws (15%); and retention clips for attaching dental prostheses to implant bars (7%). Studies on the application of PEEK as a material for the manufacture of implant healing abutments were not included in this paper, since they were considered more closely related to the surgical rather than the prosthetic aspect of the treatment.
Table 2 lists the studies involving PEEK as a framework material for IFDPs. No in vivo studies providing a control group were found; only 2 case series.20,21 Two uncontrolled clinical studies22,23 and 2 in vitro studies were identified.24,25 The prosthetic design units identified were implant-supported fixed complete dental prostheses (IFCDP); three-unit IFDPs; and single-unit IFDPs. Single-unit and three-unit IFDPs located posteriorly accounted for information regarding only fracture strength, while no information about fracture strengtwas re-corded for elements located anteriorly, nor for IFCDPs. In partial IFDPs, the failure pattern was found to be from adhesive fracture between the framework and veneering materials in all the samples tested for fracture resistance.
From the four in vivo studies reporting information on IFCDPs, 87 prostheses were identified.20–23 The weighted arithmetic means showed that, over the first 12 months following prosthetic rehabilitation, IFCDPs had a mean survival rate of 98.87% and a mean success rate of 85.05%. An incidence rate of 16% was identified for the appearance of complications over the first 12 months. Of those complications, 64.28% were found to be of a mechanical nature, while 35.72% were biologic.
Among the mechanical complications, 77.8% involved adhesive fracture between the framework and the veneering materials, 11.1% involved fracture of the framework material, and 11.1% were reports of discoloration of the prosthesis. Among the biologic complications were the appearance of soft tissue lesions and unpleasant taste.
Table 2 PEEK as IFDP Framework Material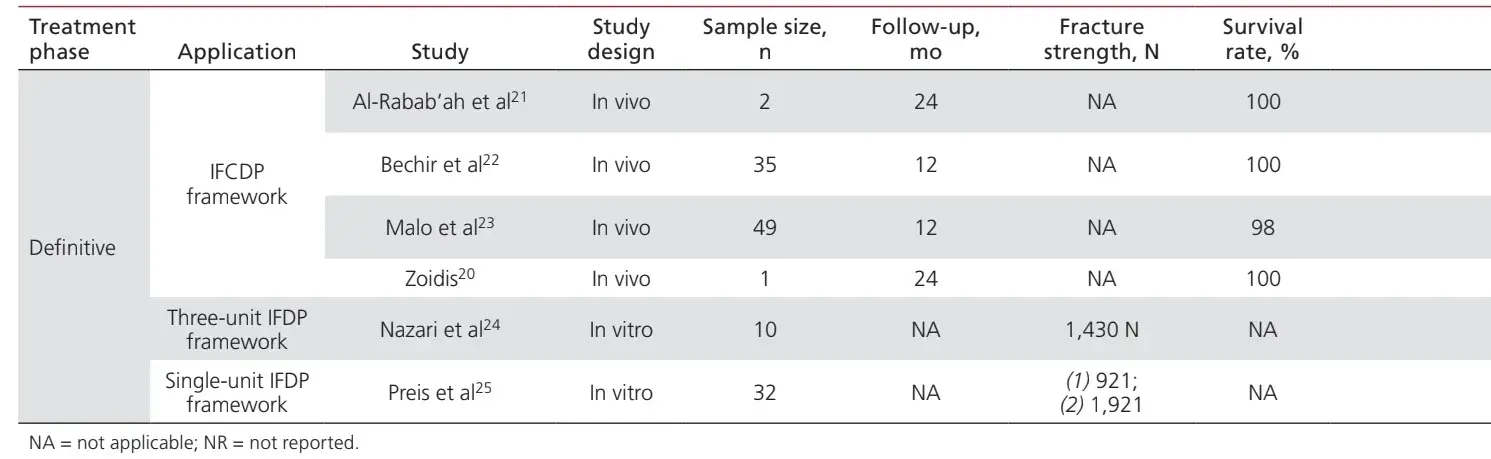
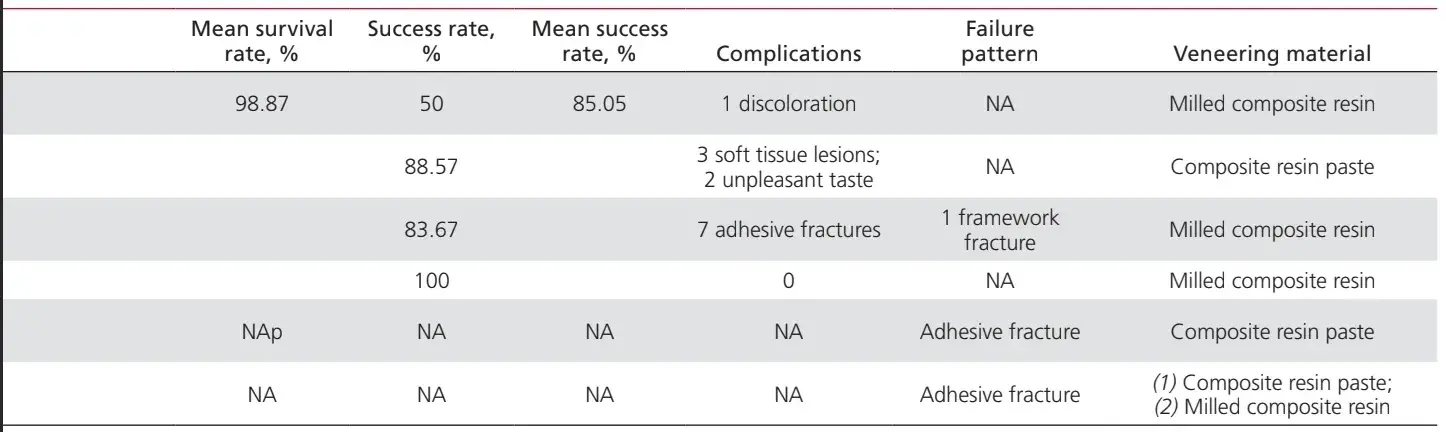
Table 3 lists the studies that discuss PEEK applications as a prosthetic implant abutment material. One case report was identified for the application of PEEK as a definitive prosthetic implant abutment,21 while two in vitro studies and two clinical studies were identified for PEEK interim prosthetic implant abutments.26–29 The use of PEEK in a definitive titanium-reinforced resin prosthetic implant abutment had only one case report, which showed 100% survival and success rates over 24 months.21 One in vivo controlled animal study, which included 24 subjects, reported a 100% survival rate over a 2-month period where PEEK was used in an interim titanium-reinforced resin prosthetic implant abutment.29
Table 3 PEEK as Prosthetic Implant Abutment Material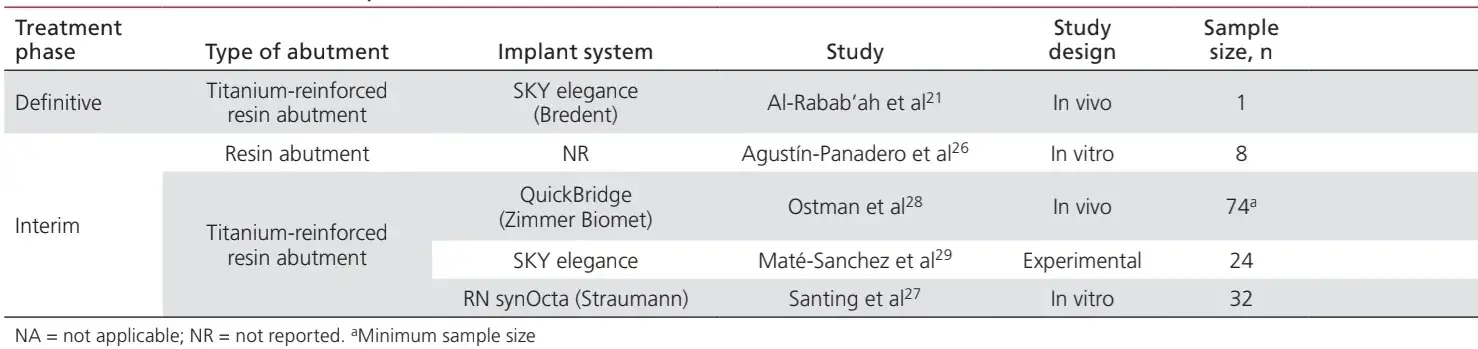
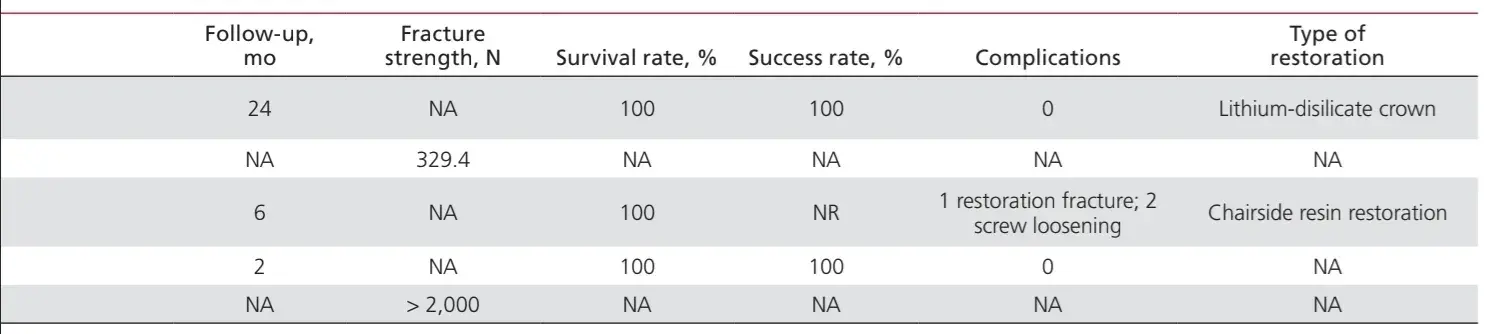
Studies involving PEEK as a material for the fabrication of implant-abutment screws and round clips for denture retention over implant bars are listed in Table 4. Only two in vitro studies concerning PEEK as an implant-abutment screw material were found.6,7 Using PEEK for retention clips to attach the prosthesis to round implant bars was discussed in only one randomized clinical trial, which showed 100% success and survival rates over the first 6 months.30
Table 4 Other PEEK Applications in Implant Prosthodontics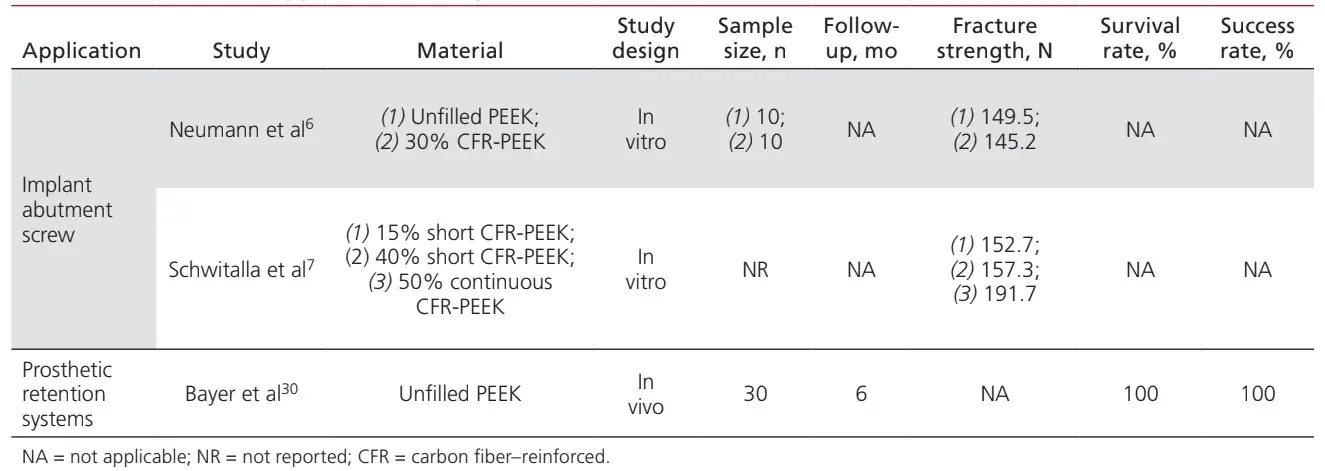
DISCUSSION
The limitations of this review include the search strategy selected for the analyzed databases, which was intentionally designed to be more general, as one of the objectives was to identify all possible applications of the material in the field of interest. For the same reason, another limitation relating to reproducibility of the online search may be the inclusion of Google Scholar among the analyzed databases. Its search algorithms often lead to wide amounts of results; however, this made it possible to map the literature not indexed in the other databases searched in this review. According to the evidence obtained, PEEK applications in implant prosthodontics may be summarized as follows.
IFDP Material
The role of PEEK as an IFDP component was the one reported most often. All of the studies that discussed PEEK as a definitive IFDP material applied the polymer to the manufacture of frameworks, which were subsequently veneered with resin materials.20–25
The resistance to fracture of PEEK IFDPs has been described as inferior to nickel-chromium [AU: “nickel-chromium” correct here?] and zirconia, but clinically acceptable. However, it should be mentioned that the information reported by the in vitro studies included in this review refers to static fatigue loads, and no information has been provided about their performance under cyclic fatigue stress, which is a more relevant indicator for the behavior of oral rehabilitations. The fabrication design and type of resin veneer also impacted the resistance to fracture, favoring cemented restorations over screw-retained ones and veneering with milled composite resin over composite paste.25,31 [AU: Sentence OK as edited?] Therefore, in situations where the choice of screw-retained or cemented designs are equally indicated, cemented restorations are believed to account for better mechanical performance, and regarding choice of veneering procedure and material, milled composite resin should be preferred. Different fabrication procedures have also been shown to influence the mechanical properties of the prosthesis. Restorations manufactured using CAD/CAM–milled PEEK appear to be more resistant to fracture than elements made using other fabrication methods.32
IFCDPs have been shown to provide highly successful treatment for patients with edentulism.33 PEEK IFCDPs may offer a reasonable meeting point between the affordability and ease of repair of metal-acrylic IFDPs and the better mechanical performance of zirconia and metal-porcelain IFCDPs.34–36
Despite the limited number of cases reported, based on the results discussed in this review, PEEK IFCDPs seem to have satisfactory survival rates (98.87%) at 12 months. Besides the fact that this statement is based on only four studies, it should also be noted that all of the included studies present short follow-up periods; however, the results are comparable to those achieved by metal-acrylic, metal-porcelain, and zirconia IFCDPs.33–35
On the other hand, the success rates for PEEK IFCDPs showed more alarming data, as a 16% incidence rate for the appearance of complications was observed at 12 months. Resin-veneered polymethyl methacrylate (PMMA) and ceramic-veneered zirconia IFCDPs were reported as showing annual complication rates of 6.6% with a 90.6% survival rate, free of complications, at 12 months.37 These figures suggest that PEEK IFCDPs incur greater risk. The incidence of complications reported here, however, should be interpreted considering certain limitations—namely, only 87 PEEK IFCDPs were identified, with a follow-up at 12 months for 84 prostheses and at 24 months for 3 prostheses. Besides the limited number of cases, the 12-month follow-up period provides limited clinical significance in the case of definitive prostheses.
Biologic complications, which were unpleasant taste and soft tissue lesions, made up 35.72% of the total cases observed. However, it should be noted that the authors of the study reporting taste alterations stated that some of the patients were also suffering from systemic conditions at the time of evaluation,22 thus adding another level of bias to the incidence rate for complications. PEEK has been previously appointed as a bioinert material38; however, Trindade et al recently observed that this material triggers higher immune activation with respect to titanium during the process of osseointegration.39 The authors suggested that the knowledge of the material’s chemical inertia was most likely based on in vitro studies, since information regarding the role of the immune system in the downregulation of the inflammatory process during the PEEK-host interaction was not available.40 It is not yet clear whether the soft tissue lesions observed in this review may be related to PEEK’s interaction with the host tissues or to confounding factors from the designs of the included studies; however, in light of the results mentioned above, this might be worthy of further investigation.
Regarding mechanical failures, 77.8% consisted of adhesive fracture between the framework and veneering materials. Failure patterns in single- and multi-unit IFDPs also mostly consisted of adhesive fractures between the framework and veneering material,24,25,31 which corroborates the findings observed for IFCDPs. This should indicate satisfactory resistance for the framework, even though, to date, no durable and predictable bonding strategy between a PEEK framework and composite veneer has been found. Future investigations should focus on finding the right balance between supplementing the PEEK formula with fillers and choosing the right surface conditioning-protocol and veneering procedure to obtain optimal mechanical performance.
Implant Abutment Material
Several in vitro and in vivo studies reported using prosthetic implant abutments composed entirely or partially of PEEK.21,27–29,41–48 However, only five studies discussed abutment-related variables that were of interest for this paper.21,26–29
In terms of mechanical performance, PEEK resin implant abutments have been described as significantly less resistant to fracture than titanium abutments.26
Their higher shock absorption capability does not negatively affect stress distribution in the implant or the peripheral bone when compared to other restoration and abutment materials.44 Nevertheless, these abutments showed higher stress concentration in the restoration crowns, which is especially relevant in the case of central incisors where the restoration is thinner, thus suggesting that PEEK resin implant abutments may require specific precautions when it comes to the design of a crown restoration.27,44
PEEK titanium-reinforced resin implant abutments have been used in cases of immediate loading by several authors.21,28 These systems are composed of a titanium core and an overlying PEEK sleeve, which may be removable or not, depending on the design of the element. More recently, an abutment composed of a titanium core with a ceramic-reinforced PEEK sleeve has been introduced to the market.21 Even if supported by only one animal study, the evidence seems to indicate that this abutment is superior to titanium in terms of soft tissue adaptation. This abutment is also suitable for the “one abutment—one time” concept, meaning that titanium-reinforced PEEK abutments could also be used as both provisional and definitive abutments.29
An in vitro study conducted by Santing et al reported that composite resin crowns supported by titanium-reinforced PEEK abutments are capable of bearing static loads up to 2,000 N.27.
Among the limitations of this paper was the impossibility to estimate success and survival rates for PEEK prosthetic implant abutments due to the paucity of in vivo information and the heterogeneity of the systems identified. However, it can be deduced from the results that PEEK titanium-reinforced implant abutments could provide superior results in terms of mechanical resistance when applied as either an interim or a definitive abutment. Therefore, use of a titanium core is preferred to the resin-only version of the component. The thickness and manufacturing process of the interim restoration could be more significant to the outcome of treatment with PEEK abutments than they would be for titanium abutments. Future research should focus on the mechanical resistance of titanium-reinforced PEEK abutments, as well as long-term in vivo outcomes.
Implant Abutment Screws
The proportional advantages given by PEEK abutment screws are related to their shock absorption properties, as well as their easier removal in case of fracture due to their lower friction coefficients. When tested for fracture strength compared to titanium, PEEK screws were shown to be 5 times less resistant, and no differences were found between the unfilled and carbon fiber–filled versions of the material. However, no description of the carbon fiber design was provided by the authors.6 In a more recent study, Schwitalla et al7 reported that PEEK screws filled with short carbon fibers (with a composition of up to 40%) showed similar mechanical behavior to what was reported by Neumann et al6 and also observed a 20% increase in tensile strength when the PEEK was filled with a continuous carbon fiber composition of at least 50%. It has been demonstrated that the addition of PMMA cement improves the mechanical resistance of carbon fiber–reinforced PEEK screws.49
The design of the connection between the implant and the restoration is another factor that could affect the mechanical performance of the abutment screw. Since PEEK abutment screws have a higher tendency to incur plastic deformation than titanium, the relations between different implant connections and screw designs should also be investigated further. The upcoming challenge for PEEK abutment screws will consist of finding the right balance in the filler composition in terms of quantity and structure, the abutment material, and the implant connection design. To date, scientific evidence lacks the consistency required to recommend them for clinical use.
Prosthetic Retention Systems
Plastic retention clips have been studied in several scenarios to investigate their retention of tooth-supported RDPs. They have been described as less retentive than commonly used materials such as cobalt-chromium, [AU: “cobalt-chromium” correct here?] but still retentive enough to serve their clinical purpose. PEEK resin clips have been shown to be potentially reliable as a retention clasp for anchoring tooth-supported RDPs with a 10-year service life; however, it seems that it is necessary to increase their diameter to twice that of the metal clasps in order to obtain sufficient long-term retention.50
In cases of implant-supported prostheses, there is limited evidence about using PEEK for retention clips. Bayer et al reported in a human randomized clinical trial that PEEK clips applied as retention devices over round implant bars had sufficient retentive force, with a clinically acceptable 20% retention loss after 6 months.30
A more recent high-performance polymer named polyetherketoneketone (PEKK) has been claimed to provide promising mechanical performances when compared to other members of the polyaryletherketones (PAEKs) family.51 Its favorable mechanical properties are given by a higher compression strength, an elastic modulus similar to human bone, and a higher polishing capability.52 In terms of bacterial adhesion, PEKK has also been demostrated to provide comparable results to conventional PEEK.53 PEKK is currently indicated for producing retention devices for implant-supported overdentures.54 Further investigations are needed to gain a better understanding of this material’s biocompatibility and feasibility for implant prosthetic treatments.
Further research is also needed to clarify diameter- and shape-related specifications for different designs of implant bars, as well as their long-term retention capability since, to date, these parameters are still unknown.
You have the opportunity to gather more in-depth information about implant-supported prosthetics in our course "Occlusion and implants".
CONCLUSIONS
Despite PEEK being used for the fabrication of several components involved in implant prosthodontic rehabilitation, the scientific evidence available is limited in quantity and quality. The lack of evidence means that undertaking a systematic review is not appropriate or necessary, but advocates further, better designed clinical research. The use of PEEK in implant prosthodontics should not yet be endorsed; however, if used, clinicians should heed the suggested protocols regarding this choice of prosthetic component, as well as its fabrication procedure and veneering material or overlying restoration, bearing in mind that long-term outcomes are still uncertain.
Authors:
Andrea Paratelli, Giammarco Perrone, Rocío Ortega, Miguel Gómez-Polo
References
Kurtz SM, Devine JN. PEEK biomaterials in trauma, orthopedic, and spinal implants. Biomaterials 2007;28:4845–4869.
Panayotov IV, Orti V, Cuisinier F, Yachouh J. Polyetheretherketone (PEEK) for medical applications. J Mater Sci Mater Med 2016;27:118.
Abu Bakar K, Cheang P, Khor K. Mechanical properties of injection molded hydroxyapatite- polyetheretherketone biocomposites. Composites Sci Technol 2003;65:421-425.
Almasi D, Iqbal N, Sadeghi M, Sudin I, Abdul Kadir MR, Kamarul T. Preparation methods for improving PEEK’s bioactivity for orthopedic and dental application: A review. Int J Biomater 2016;2016:8202653.
Suess O, Schomaker M, Cabraja M, Danne M, Kombos T, Hanna M. Empty polyetheretherketone (PEEK) cages in anterior cervical diskectomy and fusion (ACDF) show slow radiographic fusion that reduces clinical improvement: Results from the prospective multicenter “PIERCE-PEEK” study. Patient Saf Surg 2017;11:12.
Neumann EAF, Villar CC, França FM. Fracture resistance of abutment screws made of titanium, polyetheretherketone, and carbon fiber-reinforced polyetheretherketone. Braz Oral Res 2014;28:S1806-83242014000100239.
Schwitalla AD, Abou-Emara M, Zimmermann T, et al. The applicability of PEEK-based abutment screws. J Mech Behav Biomed Mater 2016;63:244–251.
Wiesli MG, Özcan M. High-performance polymers and their potential application as medical and oral implant materials: A review. Implant Dent 2015;24:448–457.
Skirbutis D, Dzingutė A, Masili naitė V, Sulcaite G, Žilinskas J. A review of PEEK polymer’s properties and its use in prosthodontics. Stomatologija 2017;19:19–23.
Najeeb S, Zafar MS, Khurshid Z, Siddiqui F. Applications of polyetheretherketone (PEEK) in oral implantology and prosthodontics. J Prosthodont Res 2016;60:12–19.
Najeeb S, Bds ZK, Bds SZ, Bds MS. Bioactivity and osseointegration of PEEK are inferior to those of titanium: A systematic review. J Oral Implantol 2016;42:512–516.
Manolea HO, Ob dan F, Popescu SM, Rîc R, M rėėescu P, Iliescu AA, et al. Current options of making implant supported prosthetic restorations to mitigate the impact of occlusal forces. Defect and Diffusion Forum 2017;376:66–77.
Georgiev J, Vlahova A, Kissov H, Aleksandrov S, Kazakova R. Possible application of BioHPP in prosthetic dentistry: A literature review. J IMAB 2018;24:1896–1898.
Schwitalla A, Müller WD. PEEK dental implants: A review of the literature. J Oral Implantol 2013;39:743–749.
Schwitalla AD, Spintig T, Kallage I, Müller WD. Pressure behavior of different PEEK materials for dental implants. J Mech Behav Biomed Mater 2016;54:295–304.
Zoidis P, Papathanasiou I. Modified PEEK resin-bonded fixed dental prosthesis as an interim restoration after implant placement. J Prosthet Dent 2016;116:637–641.
Haddaway NR, Collins AM, Coughlin D, Kirk S. The role of Google Scholar in evidence reviews and its applicability to grey literature searching. PLoS One 2015;10:e0138237.
Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med 2018;169:467–473.
Pjetursson BE, Brägger U, Lang NP, Zwahlen M. Comparison of survival and complication rates for tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs). Clin Oral Implant Res 2007;18(suppl 3):97–113.
Zoidis P. The all-on-4 modified polyetheretherketone treatment approach: A clinical report. J Prosthet Dent 2018;119:516–521.
Al-Rabab’ah M, Hamadneh W, Alsalem I, Khraisat A, Abu Karaky A. Use of high performance polymers as dental implant abutments and frameworks: A case series report. J Prosthodont 2019;28:365–372.
Bechir ES, Bechir A, Gioga C, Manu R, Burcea A, Dascalu IT. The advantages of BioHPP polymer as superstructure material in oral implantology. Mater Plast 2016;53:394–398.
Malo P, de Araújo Nobre M, Moura Guedes C, et al. Short-term report of an ongoing prospective cohort study evaluating the outcome of full-arch implant-supported fixed hybrid polyetheretherketone-acrylic resin prostheses and the All-on-Four concept. Clin Implant Dent Relat Res 2018;20:692–702.
Nazari V, Ghodsi S, Alikhasi M, Sahebi M, Shamshiri AR. Fracture strength of three-unit implant supported fixed partial dentures with excessive crown height fabricated from different materials. J Dent (Tehran) 2016;13:400–406.
Preis V, Hahnel S, Behr M, Bein L, Rosentritt M. In-vitro fatigue and fracture testing of CAD/CAM-materials in implant-supported molar crowns. Dent Mater 2017;33:427–433.
Agustín-Panadero R, Serra-Pastor B, Roig-Vanaclocha A, Román-Rodriguez JL, Fons-Font A. Mechanical behavior of provisional implant prosthetic abutments. Med Oral Patol Oral Cir Bucal 2015;20:e94–e102.
Santing HJ, Meijer HJ, Raghoebar GM, Özcan M. Fracture strength and failure mode of maxillary implant-supported provisional single crowns: A comparison of composite resin crowns fabricated directly over PEEK abutments and solid titanium abutments. Clin Implant Dent Relat Res 2012;14:882–889.
Ostman PO, Hellman M, Sennerby L, Wennerberg A. Temporary implant-supported prosthesis for immediate loading according to a chair-side concept: Technical note and results from 37 consecutive cases. Clin Implant Dent Relat Res 2008;10:71–77.
Maté Sánchez de Val JE, Gómez-Moreno G, Pérez-Albacete Martínez C, et al. Peri-implant tissue behavior around non-titanium material: Experimental study in dogs. Ann Anat 2016;206:104–109.
Bayer S, Komor N, Kramer A, Albrecht D, Mericske-Stern R, Enkling N. Retention force of plastic clips on implant bars: A randomized controlled trial. Clin Oral Implants Res 2012;23:1377–1384.
Taufall S, Eichberger M, Schmidlin PR, Stawarczyk B. Fracture load and failure types of different veneered polyetheretherketone fixed dental prostheses. Clin Oral Investig 2016;20:2493–2500.
Stawarczyk B, Eichberger M, Uhrenbacher J, Wimmer T, Edelhoff D, Schmidlin PR. Three-unit reinforced polyetheretherketone composite FDPs: Influence of fabrication method on load-bearing capacity and failure types. Dent Mater J 2015;34:7–12.
Papaspyridakos P, Mokti M, Chen CJ, Benic GI, Gallucci GO, Chronopoulos V. Implant and prosthodontic survival rates with implant fixed complete dental prostheses in the edentulous mandible after at least 5 years: A systematic review. Clin Implant Dent Relat Res 2014;16:705–717.
Bozini H, Petridis H, Garefis K, Garefis P. A meta-analysis of prosthodontic complication rates of implant-supported fixed dental prostheses in edentulous patients after an observation period of at least 5 years. Int J Oral Maxillofac Implants 2011;26:304–318.
Bidra AS, Tischler M, Patch C. Survival of 2039 complete arch fixed implant-supported zirconia prostheses: A retrospective study. J Prosthet Dent 2018;119:220–224.
Wimmer T, Huffmann AM, Eichberger M, Schmidlin PR, Stawarczyk B. Two-body wear rate of PEEK, CAD/CAM resin composite and PMMA: Effect of specimen geometries, antagonist materials and test set-up configuration. Dent Mater 2016;32:127–136.
Tartaglia GM, Maiorana C, Gallo M, Codari M, Sforza C. Implant-supported immediately loaded full-arch rehabilitations: Comparison of resin and zirconia clinical outcomes in a 5-year retrospective follow-up study. Implant Dent 2016;25:74–82.
Johansson P, Jimbo R, Kjellin P, Currie F, Chrcanovic BR, Wennerberg A. Biomechanical evaluation and surface characterization of a nano-modified surface on PEEK implants: A study in the rabbit tibia. Int J Nanomedicine 2014;9:3903–3911.
Trindade R, Albrektsson T, Galli S, Prgomet Z, Tengvall P, Wennerberg A. Bone immune response to materials, Part I: Titanium, PEEK and copper in comparison to sham at 10 days in rabbit tibia. J Clin Med 2018;7:526.
Trindade R, Albrektsson T, Galli S, Prgomet Z, Tengvall P, Wennerberg A. Bone immune response to materials, Part II: Copper and polyetheretherketone (PEEK) compared to titanium at 10 and 28 days in rabbit tibia. J Clin Med 2019;8:814.
Etxeberria M, López-Jiménez L, Merlos A, Escuín T, Viñas M. Bacterial adhesion efficiency on implant abutments: A comparative study. Int Microbiol 2013;16:235–242.
Tetelman ED, Babbush CA. A new transitional abutment for immediate aesthetics and function. Implant Dent 2008;17:51–58.
Zafiropoulos GG, Deli G, Bartee BK, Hoffmann O. Single-tooth implant placement and loading in fresh and regenerated extraction sockets. Five-year results: A case series using two different implant designs. J Periodontol 2010;81:604–615.
Kaleli N, Sarac D, Külünk S, Özturk Ö. Effect of different restorative crown and customized abutment materials on stress distribution in single implants and peripheral bone: A three-dimensional finite element analysis study. J Prosthet Dent 2018;119:437–445.
Hahnel S, Wieser A, Lang R, Rosentritt M. Biofilm formation on the surface of modern implant abutment materials. Clin Oral Implants Res 2015;26:1297–1301.
Bressan E, Stocchero M, Jimbo R, et al. Microbial leakage at morse taper conometric prosthetic connection: An in vitro investigation. Implant Dent 2017;26:756–761.
Amato F, Polara G, Spedicato GA. Tissue dimensional changes in single-tooth immediate extraction implant placement in the esthetic zone: A retrospective clinical study. Int J Oral Maxillofac Implants 2018;33:439–447.
Maté-Sánchez de Val J, Guirado JC, Ramirez Fernandez M, et al. Clinical and experimental study of new ceramic enforced PEEK-titanium hybrid abutment placed in postextraction sockets with immediate restoration. Clin Oral Implants Res 2015;26(suppl 12):356.
Stoppie N, Van Oosterwyck H, Jansen J, Wolke J, Wevers M, Naert I. The influence of Young’s modulus of loaded implants on bone remodeling: An experimental and numerical study in the goat knee. J Biomed Mater Res A 2009;90:792–803.
Tannous F, Steiner M, Shahin R, Kern M. Retentive forces and fatigue resistance of thermoplastic resin clasps. Dent Mater 2012;28:273–278.
Keilig L, Stark H, Bourauel C. Does the material stiffness of novel high-performance polymers for fixed partial dentures influence their biomechanical behavior? Int J Prosthodont 2016;30:595–597.
Fuhrmann G, Steiner M, Freitag-Wolf S, Kern M. Resin bonding to three types of polyaryletherketones (PAEKs): Durability and influence of surface conditioning. Dent Mater 2014;30:357–363.
Wang M, Bhardwaj G, Webster TJ. Antibacterial properties of PEKK for orthopedic applications. Int J Nanomedicine 2017;12:6471–6476.
Srinivasan M, Kalberer N, Maniewicz S, Müller F. Implant-retained overdentures using an attachment with true-alignment correction: A case series.


