The effect of platelet-rich plasma as a scaffold in regeneration/revitalization endodontics of immature permanent teeth assessed using 2-dimensional radiographs and cone beam computed tomography: a randomized controlled trial
Abstract
The effect of platelet-rich plasma as a scaffold in regeneration/revitalization endodontics of immature permanent teeth assessed using 2-dimensional radiographs and cone beam computed tomography: a randomized controlled trial. International Endodontic Journal, 53, 905–921, 2020.
Aim To assess the outcomes of platelet-rich plasma as a scaffold in regenerative/revitalization endodontics (RET) using cone beam computed tomography (CBCT) and 2-dimensional radiographs.
Methodology Twenty-six healthy patients with mean age of 12.66±4.47, and immature permanent anterior teeth with necrotic pulps, were randomly allocated to two groups, whereby RET was performed using platelet-rich plasma (PRP, test group) and blood clot (BLC, control group). Changes in root length (RL), root dentinal thickness (RDT), apical foramen width (AFW) and radiographic root area (RRA), were assessed using both radiographic methods, whilst changes in periapical area diameter (PAD) were assessed using CBCT, over a period of 12 months. T-test and chi-square/Fisher’s exact tests were used to compare continuous and categorical data between BLC and PRP groups, respectively. Changes in RL, RDT, AFW, RRA and PAD were examined by comparing the two groups (PRP versus BLC) using multilevel modelling, considering the clustering effect of repeated measures of several teeth originating from the same participant.
Results Changes in RL, RDT, AFW, RRA and PAD, over time, were found to be significant for both groups. There was, however, no difference between the RET techniques (PRP versus BLC), using both radiographic and CBCT methods. The results of both assessment techniques (CBCT and 2-dimensional radiographic methods) were highly consistent (overall ICC ranged between 0.80 and 0.94). In addition, a significant effect of baseline PAD was found on RL, RRA and AD at 12 months (RL effect = 0.68, P < 0.001; RRA effect = 1.91, P = 0.025; AD effect = 0.08, P = 0.024).
Conclusion The current study highlights successful and comparable clinical and radiographic outcomes of RET techniques using PRP and BLC. Standardized and calibrated 2-dimensional radiographic assessment was as effective as CBCT in assessing RET outcomes; therefore, the routine use of CBCT in RET is not recommended. Although an effect of baseline periapical lesion diameter on root development outcomes, at 12 months, were observed, more studies are recommended in order to assess such an effect.
Further details about severely damaged teeth are accessible for you to learn in our course "Saving hopeless teeth: surgical and conservative protocols".
Introduction
The use of regenerative/revitalization endodontic techniques (RET) has gained popularity in the past decade with several endodontic and paediatric dentistry organizations recognizing them as a viable management technique for immature permanent teeth with necrotic pulps (American Association of Endodontics 2013, European Society of Endodontology 2016, Duggal et al. 2017). Albeit inconsistent, the ability of this technique to promote root lengthening, thickening of root dentinal walls and apical closure (Table 1; Nicoloso et al. 2016, Tong et al. 2017, Torabinejad et al. 2017, Murray 2018) has provided the opportunity to offer RET to complement MTA apical plug techniques especially in immature teeth at an early stage of root development (stages 1, 2 or 3; Cvek 1992, Nazzal & Duggal 2017).
Various RET protocols have been suggested (Kontakiotis et al. 2015, Nazzal et al. 2018b) with differences mainly in the disinfection technique used (Martin et al. 2014), intracanal medicaments (Nagata et al. 2014), scaffold systems and restorative materials (Kim et al. 2018).
In order to reduce such variability, the American Association of Endodontics (2013) and European Society of Endodontology (2016) have developed evidence-based recommended protocols. These guidelines helped reduce some of the differences in the steps of RET such as EDTA and sodium hypochlorite use; however, variations in terms of intracanal medicament, sealing material and assessment tools still exist due to the lack of high-quality evidence. The use of appropriate scaffolds is an essential part of any appropriately designed tissue engineering regenerative endodontic strategy (Galler et al. 2011).
Although not considered a true scaffold system, most clinicians induce a blood clot (BLC) into the root canal system for the clot to act as a scaffold (Kontakiotis et al. 2015, Nazzal et al. 2018b). Platelet-rich plasma and platelet-rich fibrin have been used as RET scaffolds due to their rich content of platelets and important growth factors resulting in variable outcomes (Table 1). In comparison with a blood clot (which contains 95% RBCs, 5% Platelets and <1% WBCs), autologous platelet concentrates (PRP and PRF) contain higher concentration of platelets which incorporate important growth factors, such as plate- let-derived growth factor (PDGF), transforming growth factor-b (TGF-b), insulin-like growth factors (IGFs), vascular endothelial growth factor (VEGF), epidermal growth factor (EGF) and epithelial cell growth factor (ECGF) within their granules. Platelet-rich plasma (a first-generation platelet concentrate) contains 4% RBCs, 95% platelets and 1% WBCs. The platelet count in PRP clots exceeds 2 million µL1 (0.5 9 1011 platelets per unit) with 160% to 740% increase in platelet concentration compared to a blood clot. Platelet-rich fibrin, a second-generation platelet concentrate, later given the name leucocyte-PRF ‘L-PRF’ owing to its content of WBCs, provides a 210-fold increase in the platelet and fibrin concentration than the whole blood input volume (55 vol% plasma and 45 vol% formed elements ‘platelets, leucocytes, erythrocytes’; Tsay et al. 2005, Narang et al. 2015).
Radiographic outcomes of RET have been mainly assessed using 2-dimensional radiographic views (Table 1), most of which reported no significant differences between the RET-BLC and RET-PRP (Table 1).
Assessment of RET outcomes using cone beam computed tomography (CBCT), however, has only been performed by Alagl et al. (2017) who reported no differences between BLC and PRP in all outcomes except for root lengthening where a significant increase in favour of the PRP group was reported. The use of CBCT over 2-dimensional radiographic views could improve visualization of root development in three dimensions, hence it has been suggested for use in assessment of root development; however, these two techniques have not been compared for such a recommendation to be made.
Since the use of CBCT in assessing radiographic outcomes following RET has been recommended for assessing radiographic outcomes of RET, it was prudent to compare this method to that of 2-dimensional radiographs when assessing the success of PRP as a scaffold in RET in comparison with the traditional blood clot technique.
Therefore, the primary aim of this study was to assess the clinical and radiographic outcomes of PRP as a scaffold in RET of immature teeth with nonvital pulps in comparison with RET using blood clot scaf-fold utilizing a CBCT radiographic method. The secondary aim of this study was to compare the radiographic outcomes when using CBCT over 2-dimensional radiographs following RET treatment of immature teeth with nonvital pulps.
A null hypothesis of no significant differences in the clinical and radiographic outcomes of RET treated immature teeth with nonvital pulps following the use of PRP as a scaffold in comparison with a blood clot scaffold, when assed using CBCT, was postulated.
Table 1 A summary of the results reported by regenerative/revitalisation endodontic randomized controlled trials comparing RET using BLC versus PRP/PRF showing the method of radiographic assessment used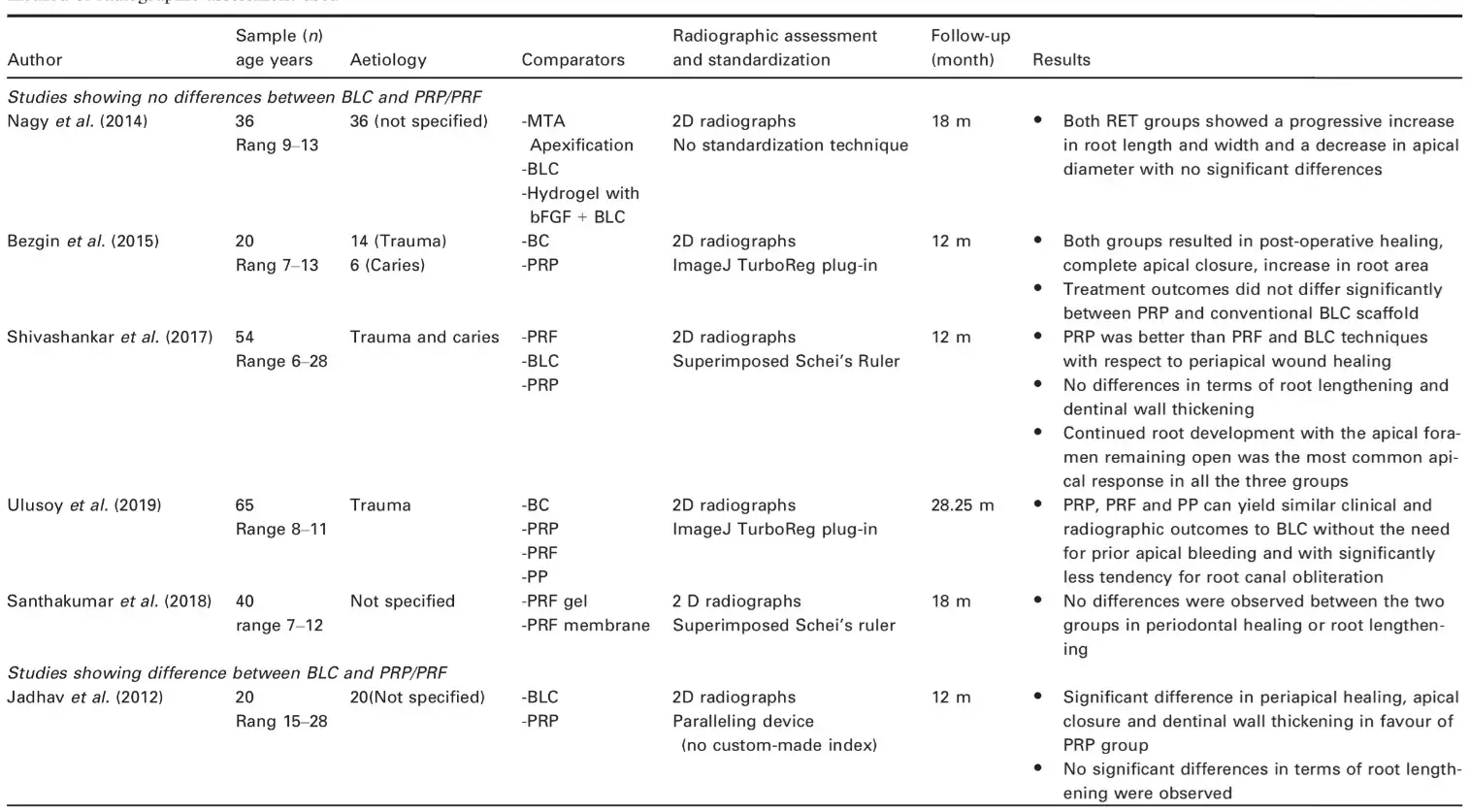
Materials and methods
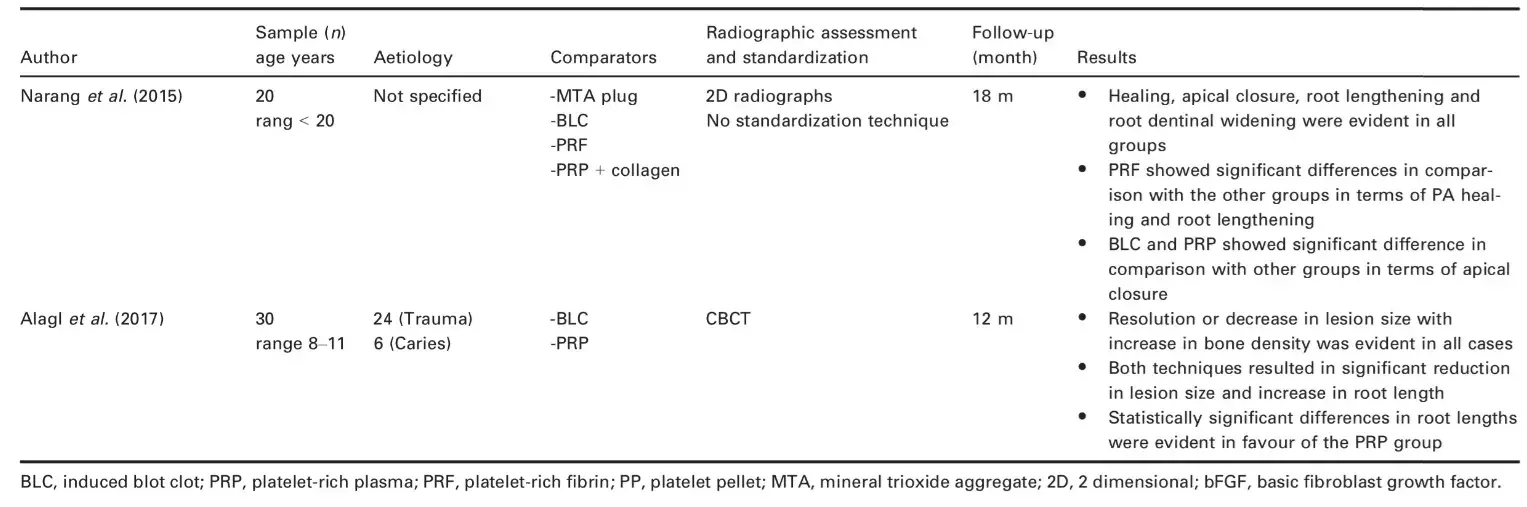
This was a randomized controlled single blinded parallel clinical trial (RCT) performed using comparative tests. Ethical approval was obtained from the ethical committee of the Faculty of Dentistry, Cairo University, Cairo, Egypt and registered at the pan African clinical trial registry [http://www.pactr.org/-PACTR ID: 201502001032409, full trial protocol is available at http://cebd.info]. This study was designed according to CONSORT guidelines for reporting randomized clinical trials (Fig. 1).
Patients attending the postgraduate outpatient clinic at the Department of Endodontics, Faculty of Dentistry, Cairo University, between January 2016 and January 2017 were approached and consented, by one of the authors (ASE), to take part in this study. At this stage, participants were informed of possible adverse effects of the proposed interventions such as crown discolouration and treatment failure.
Patients were enrolled to the present study if they fulfilled the inclusion criteria of being fit and healthy (ASA I and II), over the age of 7 years, with no learning disabilities or psychological problems, presenting with a minimum of one immature permanent anterior tooth with a nonvital pulp, and an acceptable level of cooperation. Teeth were considered immature when a minimum of 1 mm apical foramen width was evident. Those with known sensitivity or adverse reactions to medicaments or pharmaceuticals necessary for the completion of the trial, nonrestorable crowns, radiographic evidence of external or internal root resorption, root fractures and/or periodontal involvement of the affected teeth were excluded.
Participants were randomly assigned to an experimental group, in which revitalization endodontic procedures were performed using platelet-rich plasma (PRP) as a scaffold, and a control group, in which revitalization procedures were performed through initiation of bleeding (BLC) into the root canal system.
Random codes were generated using an online software (http://www.random.org/) by the Centre for Evidence-Based Dentistry in Cairo University (CEBD). The sequence codes were also concealed in opaque envelopes, by the same centre.
All procedures were performed by the same operator (ASE) as follows:
Local analgesia was delivered using Articaine 4% and 1 : 200 000 Epinephrine (Septanest, Septodont, Saint-Maur-Des-Fosses, France). Following rubber dam isolation (Sanctuary health SDN BHD, Chemor, Perak, Malaysia) and access cavity preparation, pulp tissue extirpation (partial pulp necrosis cases) was performed using barbed broaches (Mani, Inc., Utsunomiya, Tochigi, Japan) and the root canal system minimally instrumented using H-files (Mani Inc.).
Working lengths were then established using a Root ZX-II apex locator (J. Morita MFG Corporation, Fushimi-ku, Kyoto, Japan) and confirmed radiographically.
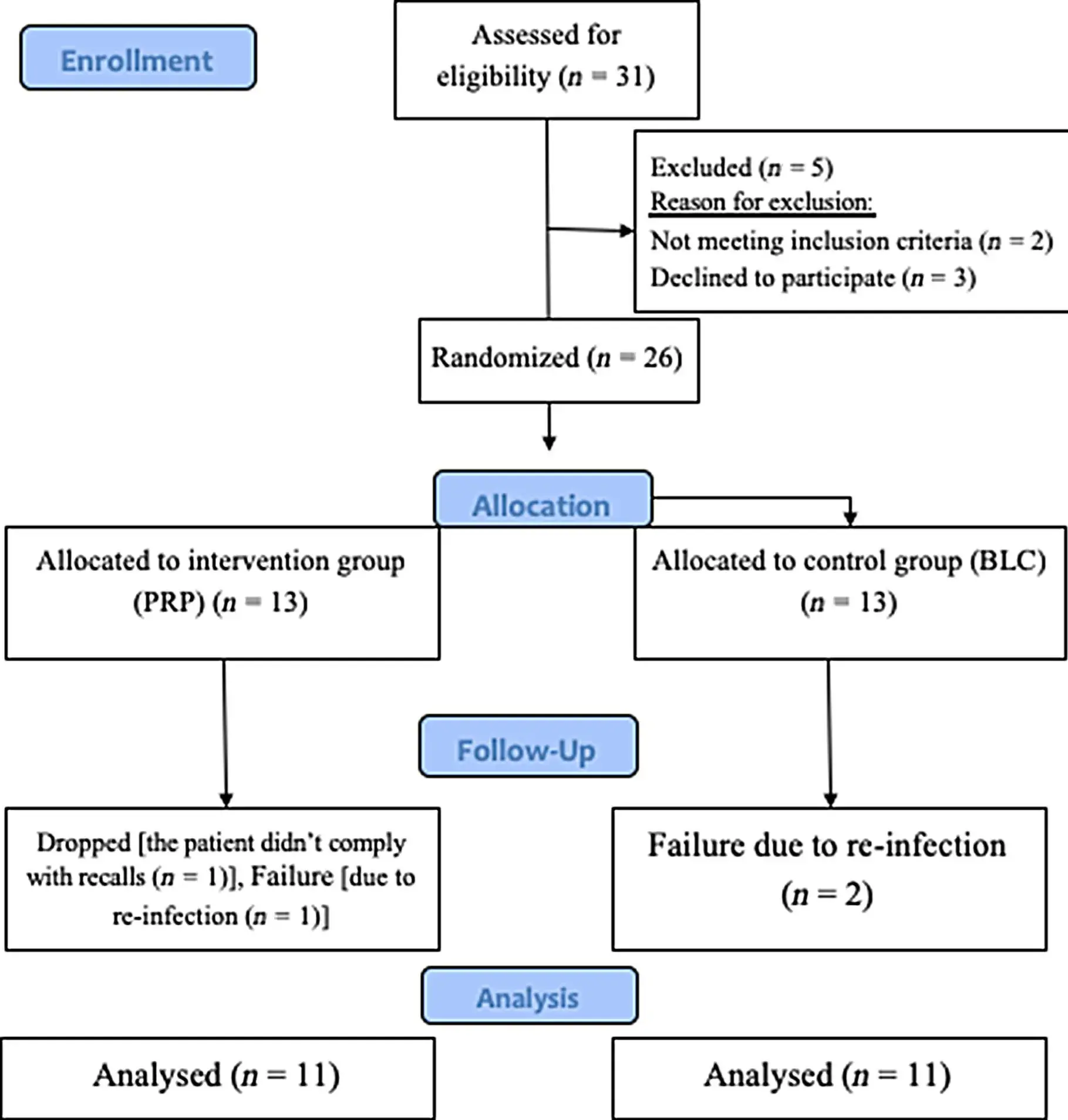 Figure 1 PRISMA flow chart showing a summary of participants enrolment, randomisation, allocation and analysis.
Figure 1 PRISMA flow chart showing a summary of participants enrolment, randomisation, allocation and analysis.
Canals were then irrigated with 20 mL of 5.25% sodium hypochlorite (NaOCl; Clorox; Nobel Wax Factories for Chemicals, Cairo, Egypt) using 0.3 mm gauge single side vented needles (Zogear products, Shanghai, China) adjusted 3 mm short of the apex.
Triple antibiotic paste, prepared according to Hoshino et al. (1996) using Minocycline (Minocin 100 mg; Wyeth Pharmaceuticals, Hangzhou, China), ciprofloxacin (Ciprocin 250 mg tablets; EPICO, Cairo, Egypt) and Metronidazole (Flagyl 500 mg tablets; Sanofi-Aventis, Cairo, Egypt) were delivered into the root canal systems using 18 G hypodermic needles (Obelis, Brussels, Belgium) and packed gently down the root canal using a hand plugger (Medesy srl, Maniago PN, Italy).
A sterile dry cotton pellet was placed over the paste after which the tooth was restored with a noneugenol containing temporary restoration (Coltosol F, Coltene/Whaledent, Altstatten, Switzerland).
Following resolution of clinical signs and symptoms of infection, local analgesia, depending on the revitalization technique described below, was delivered and teeth re-accessed and irrigated using 20 mL of 2.5% sodium hypochlorite, followed by 20 mL sterile saline and 10 mL of 17% EDTA solution (Cerkamed Dental Products, Stalowa Wola, Poland). The remainder of the treatment was dependent on the treatment group allocated as follows:
Experimental group: revitalization endodontic procedure using autologous platelet-rich plasma (RET-PRP)
Teeth in this group were anaesthetized using a local anaesthetic with vasoconstrictor (Articaine 4-% + Epinephrine 1 : 200 000; Septanest, Septodont).
Venous blood was collected, through venepuncture of the antecubital vein, into sterile glass tubes containing anticoagulant (calcium citrate). PRP was then prepared according to Dohan et al. (2006), after which concentrated platelet-rich plasma (cPRP) was prepared and introduced inside dry root canals using a sterile 30 G syringe (Dohan et al. 2006). The canal was then backfilled with cPRP to a level just beneath the CEJ and left to clot for 10 min.
Control group interventions: regenerative endodontic procedures using blood clot
Teeth, in this group, were anaesthetized using a local anaesthetic without vasoconstrictor (Scandonest 3% plain; Septodont). A pre-curved size 20 K-file (Mani Inc.) was introduced to a length 2 mm beyond the apical foramen in order to initiate bleeding, which was confirmed under magnification (18–259, Seiler Instrument Inc., St. Louis, MO, USA). A lightly moistened, sterile cotton pellet was then placed into the canal, 3-4 mm apical to the CEJ, for 7–10 min to allow blood clot formation.
Placement of the bioactive and restorative materials
After performing the regenerative/revitalization procedures assigned to each group, a collagen plug (Zimmer Biomet Inc., Lancaster, UK) was placed over the cPRP and blood clot, in order to restrict apical placement of the bioactive material. A layer of white MTA (Produits Dentaires SA, Vevey, Switzerland) was then placed over the collagen barrier followed by a moist cotton pellet and temporary restoration sealing the access cavity (Coltosol F, Coltene/Whaledent). The patients were scheduled for final restoration, after a minimum of 24 h to ensure complete setting of MTA, using a layer of reinforced glass ionomer (RIVA self-cure, SDI limited, Bayswater, Victoria, Australia) followed by resin composite (Filtek z250 universal restorative, 3 mol L1 ESPE, St. Paul, MN, USA).
Clinical and radiographic examination were performed by one operator (ASE) at baseline. Blinding of operators and patients was not possible at baseline due to the need to withdraw blood from the patients in the PRP group. A second blinded examiner (SMI), trained and calibrated, performed the clinical examination at 3, 6, 9 and 12 months from the intervention visit whilst radiographic measurements were performed by two blinded raters individually with the average used as the final measurement.
Clinical assessment
Clinical examination involved assessment of tooth colour, tenderness to percussion, presence of swellings/sinus tracts and tooth mobility. Mobility was assessed using the blunt ends of two examination mirrors, whilst basic periodontal examination (BPE; Cole et al. 2014) was performed using a graduated metal periodontal probe (Michigan O probe with Williams markings).
Pulp sensibility testing was performed using a cotton pellet, saturated with ethyl chloride (Walter ritter-GmbH pharmaceuticals, Hamburg, Germany), a small piece of hot gutta-percha, extruded from the tip of
a backfilling obturation device (Dia-Gun; Diadent international, Chungcheongbuk-do, Korea) and an electric pulp tester (EPT; Denjoy, Changsha City, Hunan Province, China).
Two-dimensional radiographic assessment
Two-dimensional radiographic examination was performed using a digital periapical radiograph and standardized using a custom-made index comprising of a Rinn film holder, a paralleling device (Dentsply Sirona, Milford, DE, USA) and silicon impressions (Aquasil, Dentsply Sirona; Fig. 2).
Mathematical image correction and calibration was performed according to Bose et al. (2009) using ImageJ software (version 1.50i; National Institutes of Health, Bethesda, MD, USA) and TurboReg plug-in (Biomedical Imaging Group, Swiss Federal Institute of Technology, Lausanne, Switzerland). Radiographic assessment involved measurement of:
Root length (RL): Measured as a straight line from the level of the tooth’s CEJ to the level of the tooth’s root apex (Fig. 3a).
Root dentinal thickness (RDT): Measured by subtracting the pulp space from the whole root thickness at 2/3 root length, in order to standardize measurements (Fig. 3b).
Apical foramen width (AFW): Measured as a line measurement from the mesial and distal root ends (Fig. 3c).
Total radiographic root area (RRA): Calculated according to (Flake et al. 2014; Fig. 3d).
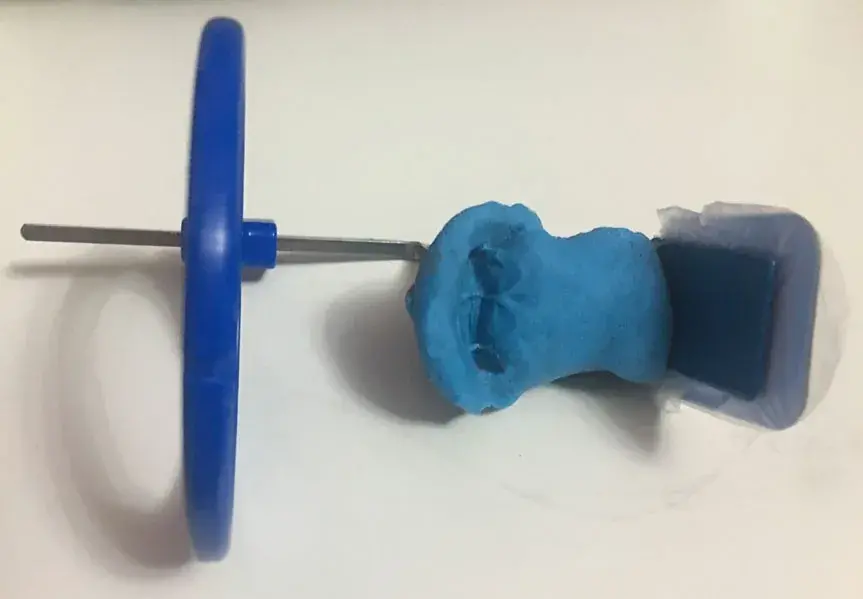 Figure 2 Custom-made index comprising of a Rinn film holder, a paralleling device (Dentsply-Sirona, USA) and silicon impressions.
Figure 2 Custom-made index comprising of a Rinn film holder, a paralleling device (Dentsply-Sirona, USA) and silicon impressions.
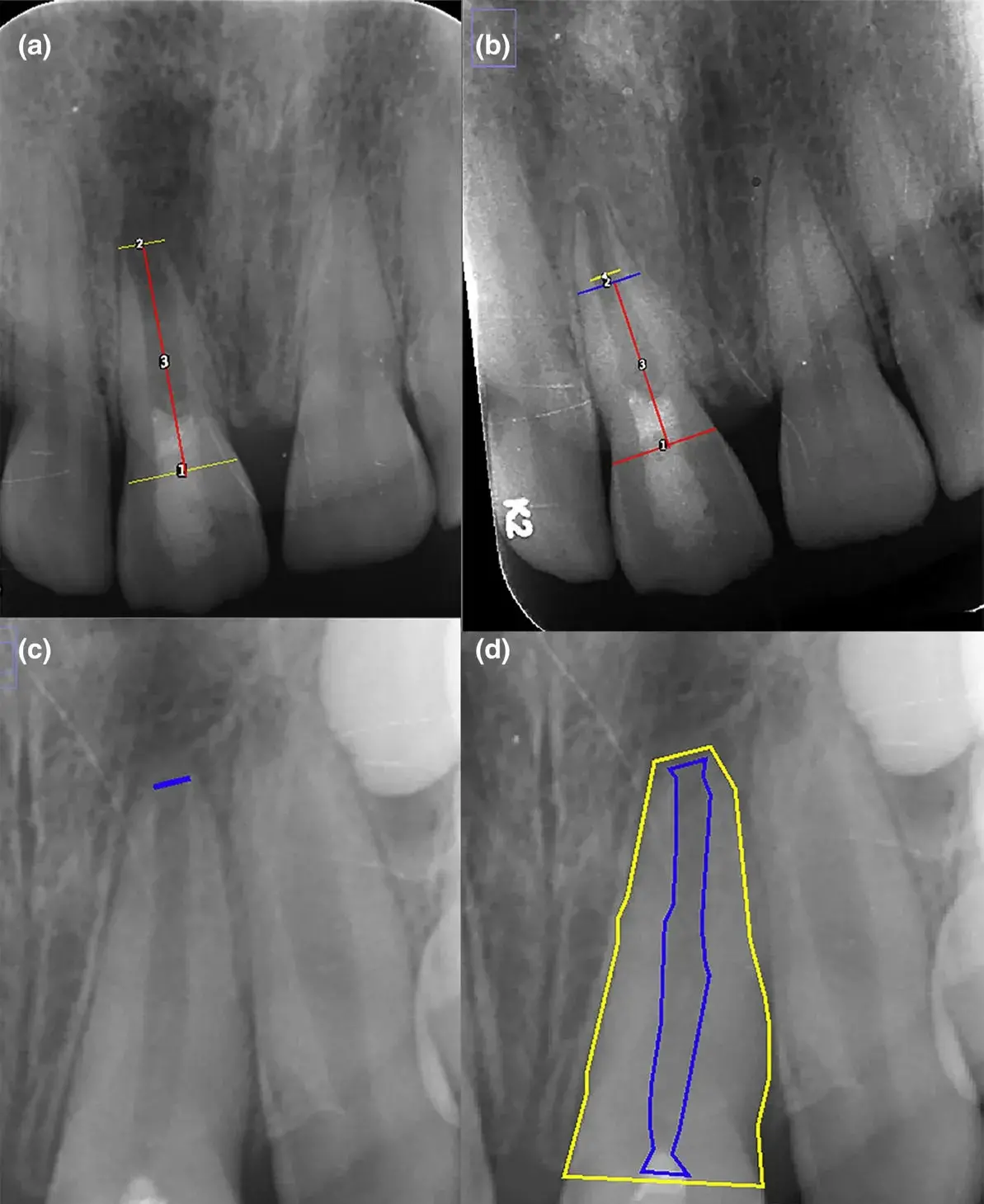 Figure 3 Periapical long cone 2D radiographs (a and c immediate post-operative images whilst b, d 12 months recall images) showing measurements of (a) An immediate post-operative radiograph showing root length measurement (a straight line (red line) from the level of the tooth’s CEJ (coronal yellow line) to the level of the tooth’s root apex (apical yellow line), (b) A 12-month radiograph showing root dentinal thickness (subtracting the pulp space (yellow line) from the whole root thickness (blue line) at 2/3 root length, in order to standardize measurements (yellow line moved slightly apically for illustration purposes), (c) immediate post-operative radiograph showing apical foramen width (a line measurement from the mesial to the distal root end), (d) A 12-month radiograph showing total radiographic root area (RRA; over all root area (area marked by yellow line) minus pulp space (area marked by blue line). The images used were for measurement illustration and do not represent the same tooth over time.
Figure 3 Periapical long cone 2D radiographs (a and c immediate post-operative images whilst b, d 12 months recall images) showing measurements of (a) An immediate post-operative radiograph showing root length measurement (a straight line (red line) from the level of the tooth’s CEJ (coronal yellow line) to the level of the tooth’s root apex (apical yellow line), (b) A 12-month radiograph showing root dentinal thickness (subtracting the pulp space (yellow line) from the whole root thickness (blue line) at 2/3 root length, in order to standardize measurements (yellow line moved slightly apically for illustration purposes), (c) immediate post-operative radiograph showing apical foramen width (a line measurement from the mesial to the distal root end), (d) A 12-month radiograph showing total radiographic root area (RRA; over all root area (area marked by yellow line) minus pulp space (area marked by blue line). The images used were for measurement illustration and do not represent the same tooth over time.
CBCT assessment
Cone beam computed tomography with limited field of view (Scanora 3D; Soredex, Tuusula, Finland) was taken at baseline and 12 months review appointments. Data were extracted using the OnDemand 3D Application (Cybermed Inc., Tustin, CA, USA). The same CBCT machine was used for all scans [90 kV–7.0 mA].
The axial planes x, y and z were used to standardize measurements. The x axial plane was parallel to the long axis of the teeth and passing across the maximum dimensions of the pulp in the bucco-lingual plane. The y axial plane was perpendicular to the x axial plane and passing across the maximum dimension of the pulp in the mesio-distal plane. The z axial plane was perpendicular to both the x and y axial planes and connected the top of the alveolar ridge crest mesially and distally to the tooth. Root length, RDT, AFW and RRA were measured in the sagittal and coronal planes with an average of the two readings taken as final scores. The technique used in measuring RL, RDT, AFW and RRA was similar to that of the 2D radiographs (Fig. 4).
In addition to the previously mentioned outcome measures, periapical area diameters (PAD), using baseline and 12-month CBCT scans, were measured using the technique described by Estrela et al. (2008).
Briefly, the lesion diameter is given based on the largest dimension of the lesion in coronal, sagittal and axial planes. The Periapical area diameter was then categorized into five scores as follows:
Score 0: PAD <=0.5 mm
Score 1: PAD of >0.5 to 1 mm
Score 2: PAD of >1 to 2 mm
Score 3: PAD of >2 to 4 mm
Score 4: PAD of >4 to 8 mm
Statistical analysis
A null hypothesis of no significant differences in clinical and radiographic outcomes, regardless of the radiographic technique used, between BLC and PRP regeneration/revitalization protocols shown over time was postulated in this study. A power calculation, based on the results of Jadhav et al. (2012), was calculated using a power of 0.8 and significance level of 0.05. Data were collected, tabulated and statistically analysed using IBM SPSS version 25 (SPSS Inc., IBM Corporation, NY, USA) for Windows and MedCalc.
Descriptive statistics were used to summarize participant’s demographics (gender, age) and characteristics of treated teeth. A t-test was used when comparing continuous data, whilst chi-square or Fisher’s exact tests were used to compare categorical data between BLC and PRP groups. Inter-rater agreement of the measurements between the two assessors had been assessed using interclass correlation for each outcome, each method, and overall measurements. Bland–Altman plots were performed to demonstrate the agreement between assessors.
The outcomes of RL, RDT, AFW and RRA, using both evaluation methods of digital radiography and CBCT, and PAD, using CBCT method, were examined by comparing the two groups (PRP versus BLC) using multilevel modelling, considering the clustering effect of repeated measures of several teeth coming from the same participant. The impact of baseline measures (RL, RDT, AFW, RRA and PAD) were adjusted in the multilevel modelling to reduce the variability of the treatment differences (Senn 2006). The baseline PAD was also adjusted in the models to assess the effect of baseline lesion diameter on RL, RDT, RRA, and AD at 12 months. Intention to teat analysis was accounted in the multilevel modelling using mixed model approach for those lost to follow-up or failed cases.
The level of agreement between the CBCT and 2-dimensional radiographic methods are assessed by intraclass correlation (ICC) at baseline and endpoint for each outcome measure. In addition, Bland–Altman plots are shown to demonstrate the agreement between CBCT and 2-dimensional radiographs. Significance level is considered at 0.05. Statistical software R was used for the analysis using ‘lme4’ packages, specifying fixed slope random intercept options.
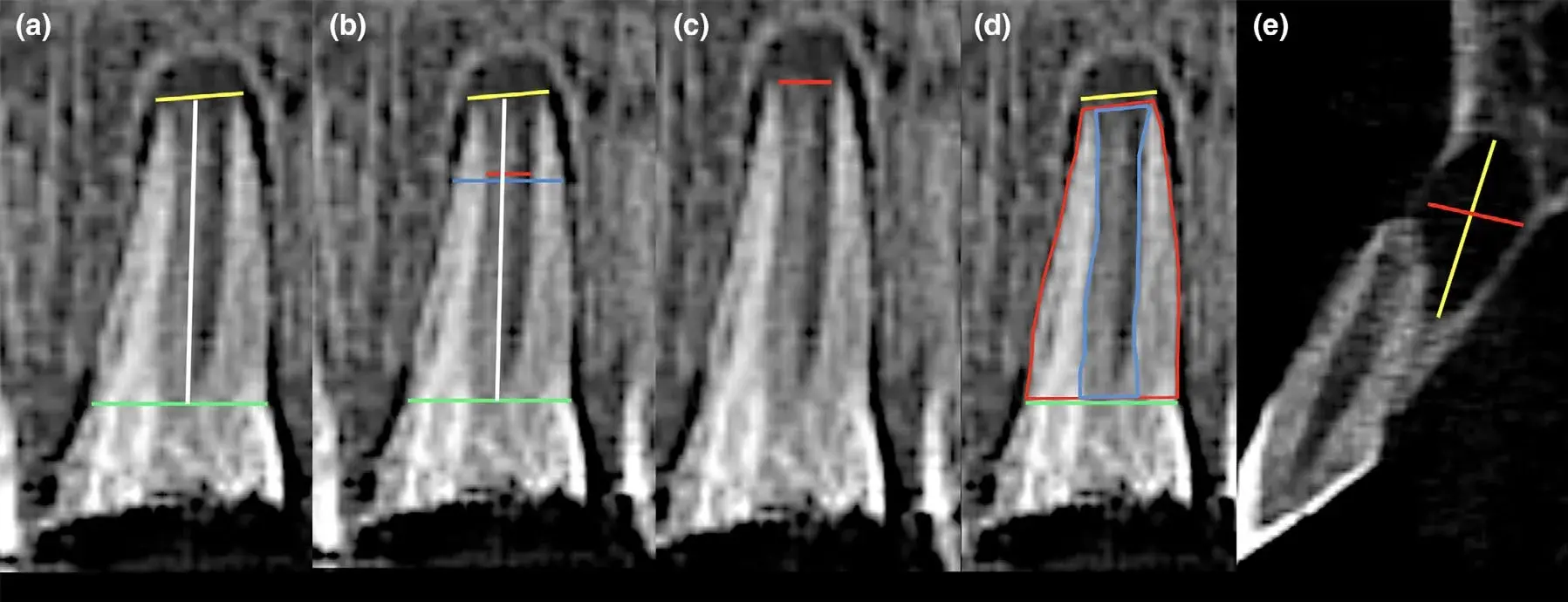 Figure 4 Pre-treatment CBCT scans in the coronal section showing measurements of (a) root length (a straight line (white line) from the level of the tooth’s CEJ (coronal green line) to the level of the tooth’s root apex (apical yellow line), (b) root dentinal thickness (subtracting the pulp space (red line) from the whole root thickness (blue line) at 2/3 root length, in order to standardize measurements, (red line moved slightly apically for illustration purposes), (c) apical foramen width (a line measurement from the mesial to the distal root end), (d) total radiographic root area (RRA; over all root area (area marked by red line) minus pulp space (area marked by blue line), (e) periapical area diameters (PAD), the lesion diameter is measured based on the largest dimension of the lesion in each plane (yellow line in comparison with the red line).
Figure 4 Pre-treatment CBCT scans in the coronal section showing measurements of (a) root length (a straight line (white line) from the level of the tooth’s CEJ (coronal green line) to the level of the tooth’s root apex (apical yellow line), (b) root dentinal thickness (subtracting the pulp space (red line) from the whole root thickness (blue line) at 2/3 root length, in order to standardize measurements, (red line moved slightly apically for illustration purposes), (c) apical foramen width (a line measurement from the mesial to the distal root end), (d) total radiographic root area (RRA; over all root area (area marked by red line) minus pulp space (area marked by blue line), (e) periapical area diameters (PAD), the lesion diameter is measured based on the largest dimension of the lesion in each plane (yellow line in comparison with the red line).
Results
The power calculation resulted in the need for 11 participants per group. Taking into consideration an expected dropout rate of 10%, an additional two participants per group were added resulting in a total sample size of 26 (13 participants per group).
No significant differences between the two groups’ (PRP and BLC) baseline patient and tooth characteristics were found (Table 2). Loss of pulp vitality was secondary to dental trauma in all cases except for one tooth in the PRP group, where loss of vitality was a result of developmental anomaly (Table 2).
All included teeth had pulpal necrosis. The presence of periapical radiolucency and swelling/sinus tract was evident in 18 (58%) and 14 (45%) of the sample, respectively (Table 2).
Table 2 Showing comparison of patient’s demographics and characteristics of treated teeth between the blood clot and PRP groups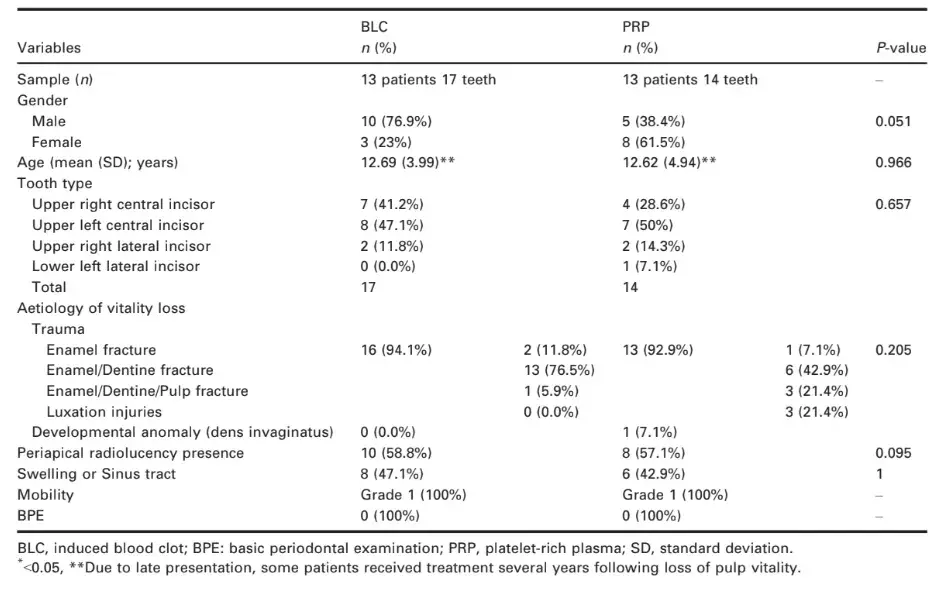
Clinical outcomes
In terms of signs and symptoms of infection, complete healing in all cases was observed at baseline and 3 months review. Only one patient (with one treated tooth) in the PRP group failed to return for second recall appointment (6 months). Two participants (each with one treated tooth) in the BLC and one participant (with one treated tooth) in the PRP group had signs of re-infection at the second recall appointment (6 months). These failed cases were treated using an MTA apical plug technique and monitored accordingly. Therefore, the overall success rate dropped to 90% [28/31 teeth; 87.1% (27/31 teeth) assuming re-infection of the case that failed to attend) at 6 months (BLC (15/17 teeth, 88%) and PRP (12/ 14 teeth, 85.7%) groups].
No change in pulp sensibility, using thermal and electric pulp testing, was observed throughout the study period with a 100% lack of response regardless of the assessment method used.
Inter-rater agreement ICC ranged from 0.997 to 1 for each dental outcome measure using PRP or BLC methods, with an overall ICC = 0.999 (95% CI = 0.999-1, P < 0.001), indicating very good agreement and consistency in measurements between the two assessors (Table 3; Fig. 5).
Table 3 Inter-rater agreement between two assessors by ICC (95% confidence interval)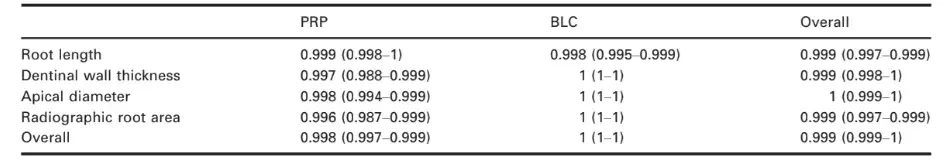
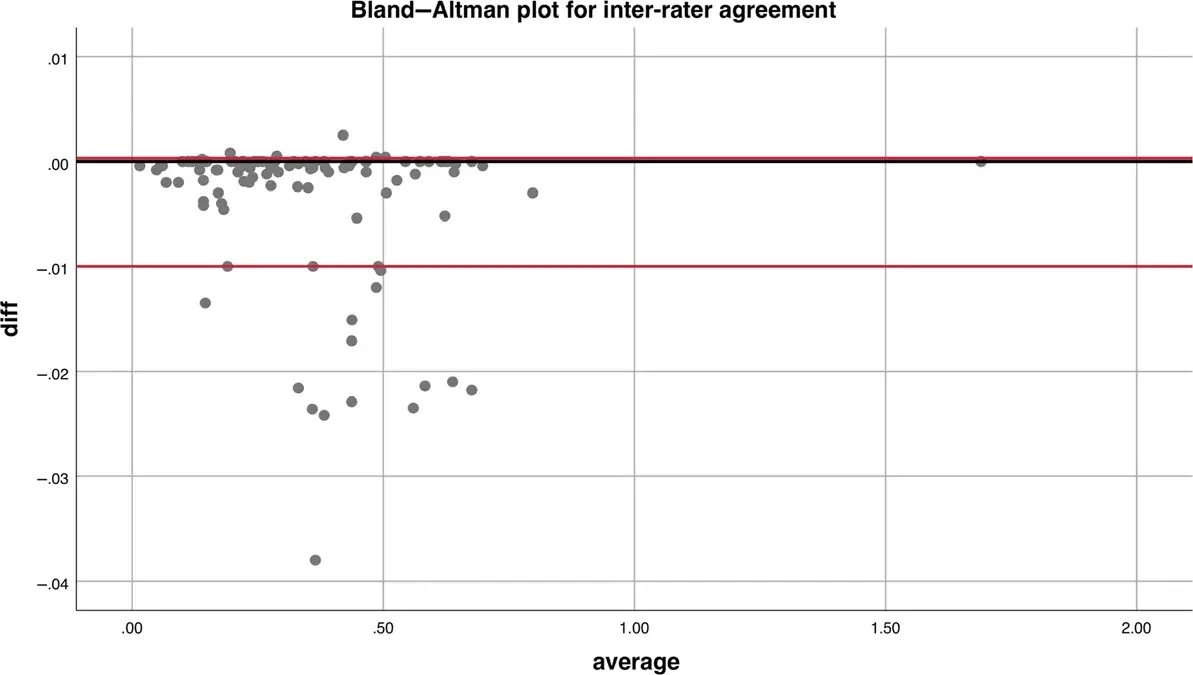 Figure 5 Bland–Altman plot showing the agreement between the two raters. Black solid line represents the reference line where zero difference is observed between the two raters, and the region between the red and the solid lines represents the range for the middle 95% observed difference values.
Figure 5 Bland–Altman plot showing the agreement between the two raters. Black solid line represents the reference line where zero difference is observed between the two raters, and the region between the red and the solid lines represents the range for the middle 95% observed difference values.
Radiographic outcomes
The group effect (PRP versus BLC) and time effect (baseline, 3, 6, 9 and 12 months) for radiographic evaluation on the four dental outcomes (RL, RDT, AFW, RRA) and CBCT methods on the five outcomes (RL, RDT, AFW, RRA and PAD) are presented in Table 4. Line plots are presented in order to illustrate time changes in each outcome measure with both radiographic assessment methods (Figs 6 and 7). Both the group effect and the time effect are adjusted by the baseline measure because the relation between baseline value and the 12-month outcomes showed significant association.
Time changes (time effect) in RL, RDT, AFW, RRA and PAD were found to be significant (P < 0.001). There was, however, no difference between the RET techniques (PRP versus BLC), using both radiographic and CBCT methods (Table 4). The results of both assessment techniques (CBCT and 2-dimensional radiographic methods) were highly consistent (Table 5; Fig. 8).
Baseline PAD had a significant effect on RL, RRA and AD at 12 months (effect = 0.68, P < 0.001, for RL; effect = 1.91, P = 0.025 for RRA; effect = 0.08, P = 0.024 for AD). The negative effect size for RL and RRA, and positive for PAD indicates that the bigger baseline PAD, the lesser the RL and RRA and the higher the PAD at 12 months.
A sensitivity analysis was performed following the removal of the one case in the PRP group where loss of pulp vitality was a result of developmental anomaly rather than trauma and showed no changes on the results reported.
Discussion
Despite the reported success of RET in terms of post-operative healing, continuation of root development has been inconsistently reported in the literature (Tong et al. 2017). Several reasons have been suggested for this inconsistency, such as the variability of RET protocols used, the lack of ideal stem cell scaffold systems, damage to Hertwig epithelial root sheath (HERS) as a result of dental trauma or long-standing periapical infection, and variability of the radiographic assessment techniques used (Nazzal & Duggal 2017, Kim et al. 2018).
The use of BLC as a RET scaffold system has been questioned as it is likely to promote healing rather than controlled pulpal regeneration (Kim et al. 2018); therefore, a more controlled scaffolding system that promotes pulp-like tissue and odontoblastic cell differentiation is needed (Galler et al. 2011, Matoug-Elwerfelli et al. 2018).
The use of platelet-rich plasma has been suggested as a more suitable scaffold system due to its rich content of platelets and important growth factors (Tsay et al. 2005, Narang et al. 2015). This scaffold system has, therefore, been extensively researched in the past decade with most studies showing no significant improvement in clinical and radiographic results to that of BLC (Table 1). Continuation of root development, in these studies, has been assessed using 2-dimensional radiographs which has also been questioned as a suitable assessment tool in RET. Changing the exposure angle of 2-dimensional radiographs, in assessing 3-dimensional root development, could result in false negative or positive results (Bose et al. 2009). To overcome such limitation, different X-ray standardization and calibration techniques, such as the use of bite blocks and image calibration software, have been reported in the literature (Table 1), however with no evidence to support one technique over the other.
Recently, the use of CBCT has been recommended as a more suitable radiographic assessment tool in RET by the American Association of Endodontics (2018). The present study, therefore, was conducted in order to assess the clinical and radiographic outcomes of PRP as a scaffold in RET using CBCT and also to assess the efficacy of using CBCT over 2-dimensional radiographs in evaluating radiographic outcomes following RET.
In the present study, both radiographic methods revealed an increase in root lengths, dentinal root widths, RRA and a decrease in AFW and PAD over time when accounting for all other confounders with no significant difference between the two scaffolds.
These results are consistent with the majority of studies comparing BLC and PRP using the 2-dimensional radiographic assessment method (Table 1). To date, only three randomized controlled trials reported differences between the two scaffolds in favour of the PRP group (Jadhav et al. 2012, Narang et al. 2015, Alagl et al. 2017). The results of these three trials, however, differed in which periapical healing, apical closure and RDT were reported to be in favour of PRP in one trial (Jadhav et al. 2012), root lengthening in favour of PRP in two trials (Narang et al. 2015, Alagl et al. 2017) and reduction in periapical areas in favour of PRP in two studies (Jadhav et al. 2012, Narang et al. 2015). Systematic reviews and meta-analyses, assessing the success of RET using BLC and PRP/ PRF, have shown an excellent chance of success, tooth survival and resolution of periapical pathosis with inconsistencies in apical closure and continued root development (Murray 2018, Metlerska et al. 2019). Such inconsistencies might be attributed to both the lack of good 2-dimensional radiograph standardization and image calibration across all included trials, as well as the potential effect on damage to the HERS following dental trauma in traumatized teeth of teeth included in these trials.
The present study is the only one comparing the use of 2-dimensional and CBCT radiographic techniques in assessing RET success. The consistency in measuring radiographic outcomes between standardized 2-dimensional and CBCT radiographic methods, reported in the present study, contradicts the current trend in recommending the CBCT method (Revised 4/1/2018). These results might be attributed to the standardization techniques used for the 2-dimensional radiographic views in which a combination of image standardization (radiographic collimators with bite registration using same radiographic settings) and image calibration using computer software (TurboReg plugin software) was used. Discouraging the routine use of CBCT in assessing RET, based on the results of the present study, is in line with the current CBCT position statements of the American Association of Endodontists (2015) and European Society of Endodontology (2019) in which the routine use of CBCT in Endodontics is discouraged. Instead, a risk–benefit analysis should be performed prior to CBCT use in any endodontic technique.
Damage to HERS as a result of dental trauma and/or long-standing infection have been hypothesized as a cause for lack of root lengthening following RET (Nazzal & Duggal 2017). Such an hypothesis was based on the lower success rates published for RET in traumatized teeth (Nagata et al. 2014, Saoud et al. 2014, Nazzal et al. 2018a) in comparison with studies presenting a mixture of traumatized and nontraumatized teeth. In addition, a recent study comparing RET in traumatized and nontraumatized teeth reported significant increase in root lengthening and thickening of dentinal walls in favour of the nontraumatized teeth treated using RET (Lin et al. 2017). Similarly, the teeth included in the present study lost vitality as a result of dental trauma, except for one case of developmental anomaly (dens invaginatus). Excluding this single case did not affect the results reported. The only study comparing BLC and PRP in traumatized teeth was that of Ulusoy et al. (2019) that agreed with the present study, in which similar clinical and radiographic outcomes of RET using PRP and BLC were reported.
Interestingly, most of the studies assessing success of RET in traumatized teeth, mainly using BLC, has shown a tendency to achieve thickening of dentinal walls and apical closure rather than root lengthening in traumatized immature teeth with nonvital pulps over a long period of time (Nazzal et al., 2019). Therefore, long-term reporting of the results of the present study is planned.
The effect of periapical lesions on the success of RET have been suggested as one of the factors leading to the inconsistent results of RET due to its potential damage to the HERS, however, such an effect has not been assessed to date. In the current study, the diameter of the baseline periapical area has been shown to affect RL, RDT, RRA and AFW at 12 months with more favourable outcomes in cases with smaller apical lesions. These results might suggest a damaging effect of more extensive periapical lesions on HERS or possibly the need for a reduction/elimination of periapical lesions prior to RET treatment. Such effects might have also contributed to the inconsistent results reported in the literature.
The release of inflammatory cytokines, such as IL-1a and TNF-b by immunoinflammatory cells, might be associated with stem cell inhibition and/or adversely affect the biological function of HERS. Such an effect might be reversible following resolution of infection.
The effect of traumatic dental injuries, on the other hand, might be more severe, therefore, resulting in irreversible damage to HERS. Further research should be conducted to assess the effect of periapical lesions and dental trauma on HERS survival and function. In addition, the effect of trauma and infection factors such as the trauma type, trauma characteristics, size of the periapical lesion and infection period of time on HERS survival should be assessed. The inability to blind the operator and patients, due to the need to withdraw blood from the PRP group, was one of the limitations of the present study.
This might have introduced some procedural bias into the study design. However, steps were introduced to reduce such bias by including a second blinded examiner from 3 months recall and blinded assessors/raters.
Another limitation to the present study was the post-operative coronal discolouration which was evident in 14 teeth (82.4%) in the BLC group and 11 teeth (78.6%) in the PRP group. The RET protocol used in this study involved the use of tri-antibiotic paste containing minocycline and nonbismuth oxide containing white MTA. The use of such material has been associated with the development of crown discolouration (Lenherr et al. 2012, Kahler & Rossi-Fedele 2016). The use of nonbismuth oxide white MTA, such as that used in the present study, has been reported to result in less crown discolouration in comparison with the more traditional MTA (Lenherr et al. 2012, Nazzal et al. 2018a, 2019). The use of biantibiotic containing no minocycline (Nazzal et al. 2018a) or tri-antibiotic paste, whereby minocycline is replaced with other antibiotics such as cefaclor (Bezgin et al. 2015), could have helped reduce the post-operative discolouration encountered in the present study.
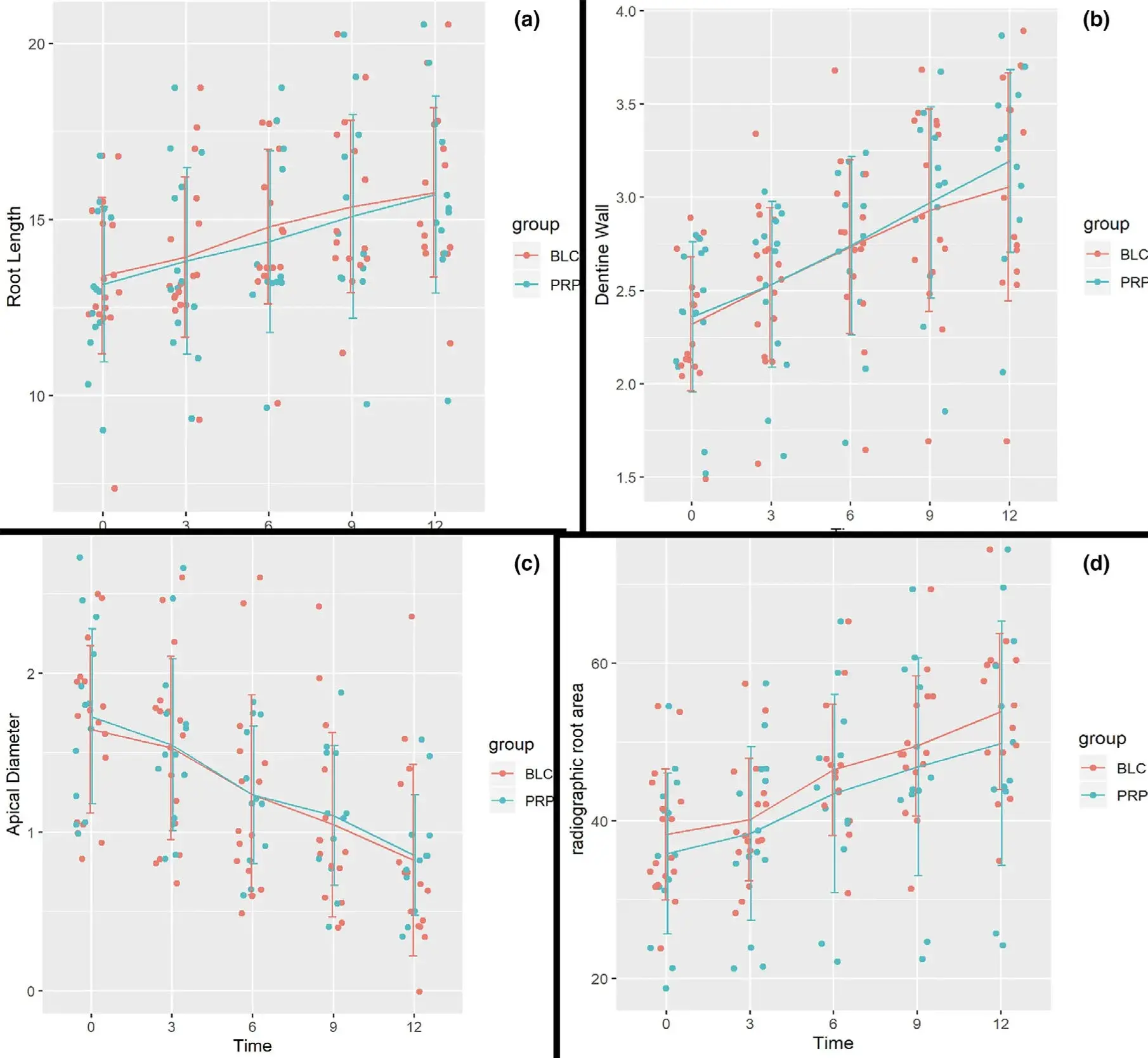 Figure 6 Change over time of the four dental outcomes (root length (a), dentinal wall thickness (b), apical foramen width (c), and radiographic root area (d)) using periapical radiographic method measured at baseline, 3, 6, 9 and 12 months
Figure 6 Change over time of the four dental outcomes (root length (a), dentinal wall thickness (b), apical foramen width (c), and radiographic root area (d)) using periapical radiographic method measured at baseline, 3, 6, 9 and 12 months
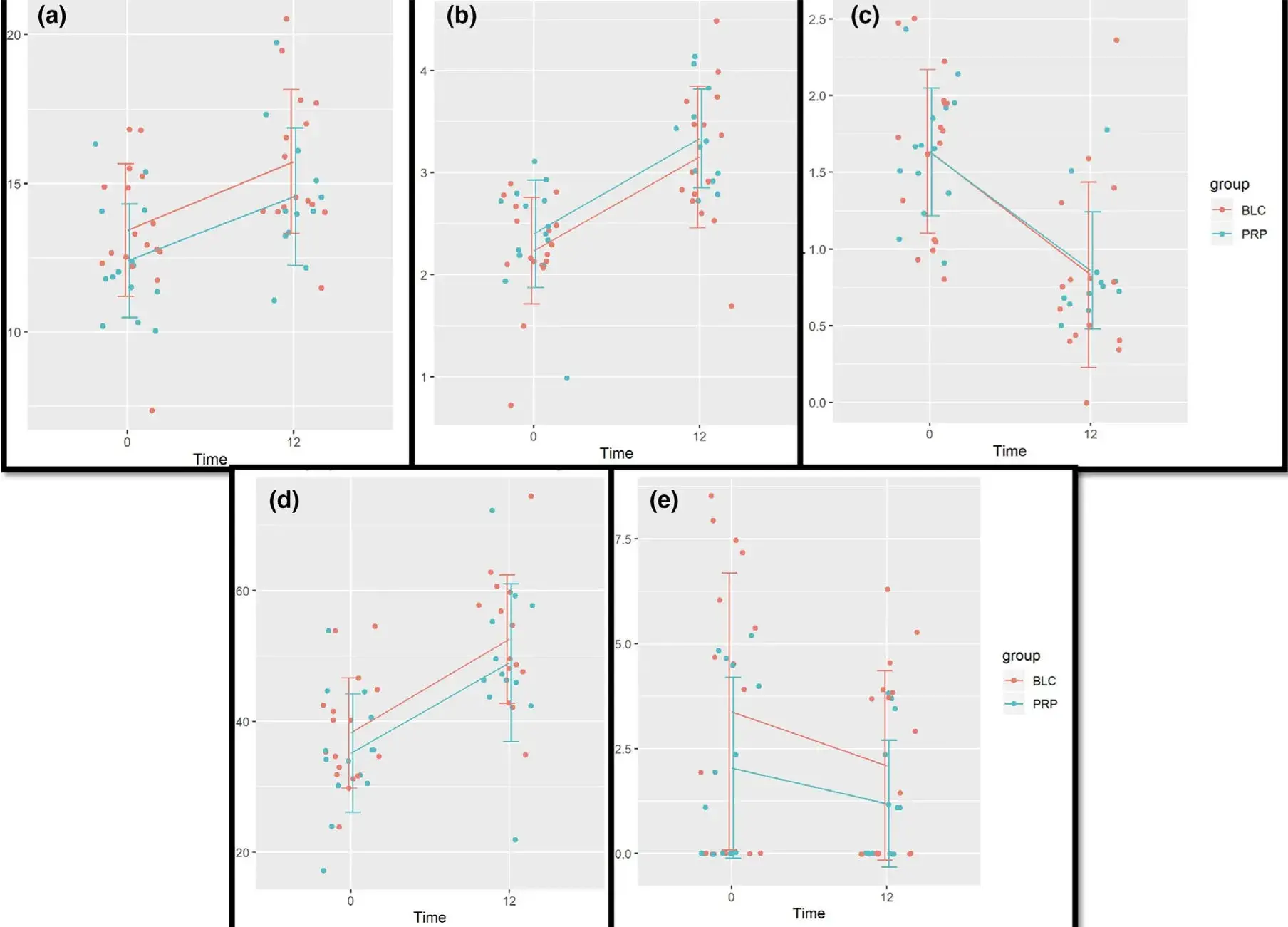 Figure 7 Change over time of the five outcomes, root length (a), dentinal wall thickness (b), apical foramen width (c), radiographic root area (d) and periapical area diameter (e) using CBCT method, measured at baseline and 12 months.
Figure 7 Change over time of the five outcomes, root length (a), dentinal wall thickness (b), apical foramen width (c), radiographic root area (d) and periapical area diameter (e) using CBCT method, measured at baseline and 12 months.
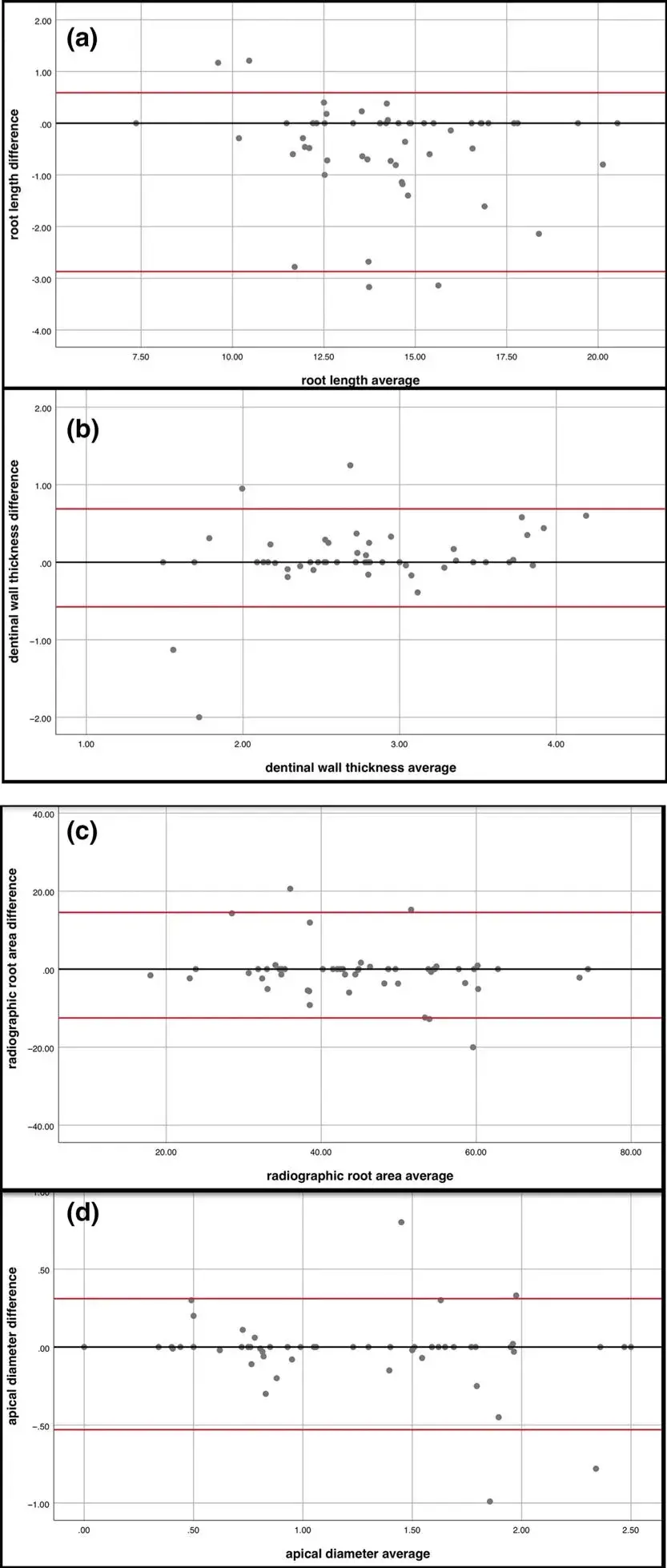 Figure 8 Bland–Altman plot showing the agreement between CBCT and 2-dimensional radiographs for root length (a), root dentine width (b), apical foramen width (c) and radiographic root area (d). Black solid line is the reference line where zero difference is observed between CBCT and radiograph, and the region between two red solid lines are the range for middle 95% observed difference values.
Figure 8 Bland–Altman plot showing the agreement between CBCT and 2-dimensional radiographs for root length (a), root dentine width (b), apical foramen width (c) and radiographic root area (d). Black solid line is the reference line where zero difference is observed between CBCT and radiograph, and the region between two red solid lines are the range for middle 95% observed difference values.
Table 4 Comparison between PRP and BLC group effect (overall difference between the two groups when all confounders are controlled) and time effects (average difference between next time and previous time, when other variables are controlled) using conventional radiographic and CBCT evaluation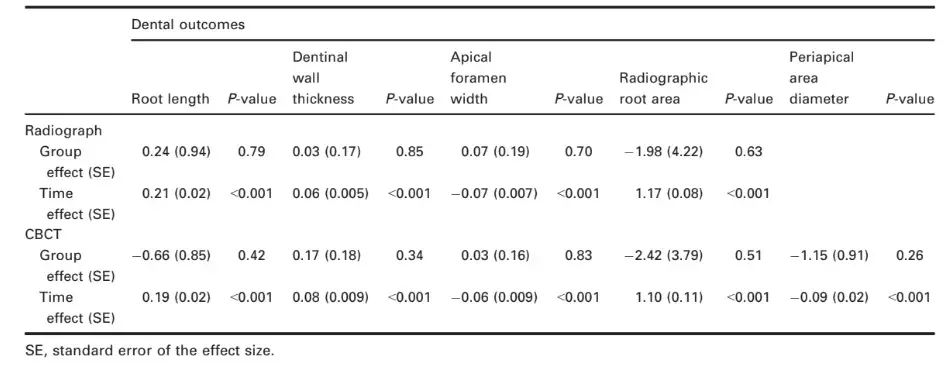
Table 5 Level of agreement between radiograph and CBCT, ICC (95% confidence interval)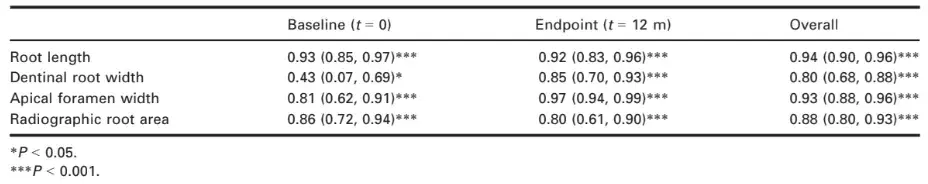
Conclusions
The results of the current study highlight:
A successful and comparable clinical and radiographic outcomes of regenerative/revitalization endodontic technique using PRP and BLC as scaffolds in immature traumatized permanent teeth with necrotic pulps over a period of 12 months.
The effectiveness of standardized and calibrated 2-dimensional radiographs in prospective assessment of RET root development parameters in comparison with CBCT. Therefore, the routine use of CBCT in RET is not recommended.
Whilst the results of the current study demon-%strate an effect of the diameter of the preoperative periapical lesion on root development outcomes at 12 months, future studies are needed in order to determine the impact of such effect.
If you enjoyed reading this article and would like to explore the endodontic treatment protocols further, we encourage you to enroll our website.
List of authors:
A. S. ElSheshtawy, H. Nazzal, O. I. El Shahawy, A. A. El Baz, S. M. Ismail, J. Kang, K. M. Ezzat
References
Alagl A, Bedi S, Hassan K, AlHumaid J (2017) Use of platelet-rich plasma for regeneration in non-vital immature permanent teeth: clinical and cone-beam computed tomography evaluation. Journal of International Medical Research 45, 583–93.
American Association of Endodontics (2013) AAE position statement: scope of endodontics-regenerative endodontics [Online]. Chicago, IL: American Association of Endodontics-AAE.
American Association of Endodontics (2018) AAE Clinical Considerations for a Regenerative Procedure.
American Association of Endodontists, The American Academy of Oral and Maxillofacial Radiology (2015) AAE and AAOMR Joint Position Statement: Use of Cone Beam Computed Tomography in Endodontics—2015/2016 Update. American Association of Endodontists position statement [Online].
Bezgin T, Yilmaz AD, Celik BN, Kolsuz ME, Sonmez H (2015) Efficacy of platelet-rich plasma as a scaffold in regenerative endodontic treatment. Journal of Endodontics 41, 36–44.
Bose R, Nummikoski P, Hargreaves K (2009) A retrospective evaluation of radiographic outcomes in immature teeth with necrotic root canal systems treated with regenerative endodontic procedures. Journal of Endodontics 35, 1343–9.
Cole E, Ray-Chaudhuri A, Vaidyanathan M, Johnson J, Sood S (2014) Simplified basic periodontal examination (BPE) in children and adolescents: a guide for general dental practitioners. Dental Update 41, 328–37.
Cvek M (1992) Prognosis of luxated non-vital maxillary incisors treated with calcium hydroxide and filled with guttapercha. A retrospective clinical study. Endodontics & Dental Traumatology 8, 45–55.
Dohan DM, Choukroun J, Diss A et al. (2006) Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontics 101, e37–44.
Duggal M, Tong HJ, Al-Ansary M, Twati W, Day PF, Nazzal H (2017) Interventions for the endodontic management of non-vital traumatised immature permanent anterior teeth in children and adolescents: a systematic review of the evidence and guidelines of the European Academy of Paediatric Dentistry. European Archives of Paediatric Dentistry 18, 139–51.
Estrela C, Bueno M, Azevedo B, Azevedo J, Pecora J (2008) A new periapical index based on cone beam computed tomography. Journal of Endodontics 34, 1325–31.
European Society of Endodontology (2016) European Society of Endodontology position statement: revitalisation procedures. International Endodontic Journal 49, 717–23.
European Society of Endodontology (2019) European Society of Endodontology position statement: Use of cone beam computed tomography in endodontics. International Endodontic Journal 52, 1675–8.
Flake NM, Gibbs JL, Diogenes A, Hargreaves KM, Khan AA (2014) A standardized novel method to measure radiographic root changes after endodontic therapy in immature teeth. Journal of Endodontics 40, 46–50.
Galler KM, D’Souza R, Hartgerink J, Schmalz G (2011) Scaffolds for dental pulp tissue engineering. Advances in Dental Research 23, 333–9.
Hoshino E, Kurihara-Ando N, Sato I et al. (1996) In-vitro antibacterial susceptibility of bacteria taken from infected root dentine to a mixture of ciprofloxacin, metronidazole and minocycline. International Endodontic Journal 29, 125–30.
Jadhav G, Shah N, Logani A (2012) Revascularization with and without platelet-rich plasma in nonvital, immature, anterior teeth: a pilot clinical study. Journal of Endodontics 38, 1581–7.
Kahler B, Rossi-Fedele G (2016) A review of tooth discoloration after regenerative endodontic therapy. Journal of Endodontics 42, 563–9.
Kim SG, Malek M, Sigurdsson A, Lin LM, Kahler B (2018) Regenerative endodontics: a comprehensive review. International Endodontic Journal 51, 1367–88.
Kontakiotis EG, Filippatos CG, Tzanetakis GN, Agrafioti A (2015) Regenerative endodontic therapy: a data analysis of clinical protocols. Journal of Endodontics 41, 146–54.
Lenherr P, Allgayer N, Weiger R, Filippi A, Attin T, Krastl G (2012) Tooth discoloration induced by endodontic materials: a laboratory study. International Endodontic Journal 45, 942–9.
Lin J, Zeng Q, Wei X et al. (2017) Regenerative endodontics versus apexification in immature permanent teeth with apical periodontitis: a prospective randomized controlled study. Journal of Endodontics 43, 1821–7.
Martin DE, De Almeida JF, Henry MA et al. (2014) Concentration-dependent effect of sodium hypochlorite on stem cells of apical papilla survival and differentiation. Journal of Endodontics 40, 51–5.
Matoug-Elwerfelli M, Duggal MS, Nazzal H, Esteves F, Raif E (2018) A biocompatible decellularized pulp scaffold for regenerative endodontics. International Endodontology Journal 51, 663–73.
Metlerska J, Fagogeni I, Nowicka A (2019) Efficacy of autologous platelet concentrates in regenerative endodontic treatment: a systematic review of human studies. Journal of Endodontics 45, 20–30.
Murray PE (2018) Platelet-rich plasma and platelet-rich fibrin can induce apical closure more frequently than bloodclot revascularization for the regeneration of immature permanent teeth: a meta-analysis of clinical efficacy. Frontiers in Bioengineering and Biotechnology 6, 139.
Nagata JY, Gomes BP, Rocha Lima TF et al. (2014) Traumatized immature teeth treated with 2 protocols of pulp revascularization. Journal of Endodontics 40, 606–12.
Nagy MM, Tawfik HE, Hashem AA, Abu-Seida AM (2014) Regenerative potential of immature permanent teeth with necrotic pulps after different regenerative protocols. Journal of Endodontics 40, 192–8.
Narang I, Mittal N, Mishra N (2015) A comparative evaluation of the blood clot, platelet-rich plasma, and platelet-rich fibrin in regeneration of necrotic immature permanent teeth: a clinical study. Contemporary Clinical Dentistry 6, 63–8.
Nazzal H, Duggal MS (2017) Regenerative endodontics: a true paradigm shift or a bandwagon about to be derailed? European Archives of Paediatric Dentistry 18, 3–15.
Nazzal H, Kenny K, Altimimi A, Kang J, Duggal MS (2018a) A prospective clinical study of regenerative endodontic treatment of traumatised immature teeth with necrotic pulps using bi-antibiotic paste. International Endodontic Journal 51(Suppl. 3), e204–15.
Nazzal H, Tong H, Nixon P, Duggal M (2018b) Regenerative endodontic therapy for managing immature non-vital teeth: a national survey of UK paediatric dental specialists and trainees. British Dental Journal 224, 247–54.
Nazzal H, Ainscough S, Kang J, Duggal MS (2019) Revitalisation endodontic treatment of traumatised immature teeth: a prospective long-term clinical study. European Archives of Paediatric Dentistry.
Nicoloso GF, Potter IG, Rocha RO, Montagner F, Casagrande L (2016) A comparative evaluation of endodontic treatments for immature necrotic permanent teeth based on clinical and radiographic outcomes: a systematic review and meta-analysis. International Journal of Paediatric Dentistry 27, 217–27.
Santhakumar M, Yayathi S, Retnakumari N et al. (2018) A clinicoradiographic comparison of the effects of platelet-rich fibrin gel and platelet-rich fibrin membrane as scaffolds in the apexification treatment of young permanent teeth. Journal of the Indian Society of Pedodontics and Preventive Dentistry 36, 65–70.
Saoud TM, Zaazou A, Nabil A, Moussa S, Lin LM, Gibbs JL (2014) Clinical and radiographic outcomes of traumatized immature permanent necrotic teeth after revascularization/revitalization therapy. Journal of Endodontics 40, 1946–52.
Senn S (2006) Change from baseline and analysis of covariance revisited. Statistics in Medicine 24, 4334–44.
Shivashankar VY, Johns DA, Maroli RK et al. (2017) Comparison of the effect of PRP, PRF and induced bleeding in the revascularization of teeth with necrotic pulp and open apex: a triple blind randomized clinical trial. Journal of Clinical and Diagnostic Research 11, ZC34–ZC9.
Tong HJ, Rajan S, Bhujel N, Kang J, Duggal M, Nazzal H (2017) Regenerative endodontic therapy in the management of nonvital immature permanent teeth: a systematic review- outcome evaluation and meta-analysis. Journal of Endodontics 43, 1453–64.
Torabinejad M, Nosrat A, Verma P, Udochukwu O (2017) Regenerative endodontic treatment or mineral trioxide aggregate apical plug in teeth with necrotic pulps and open apices: a systematic review and meta-analysis. Journal of Endodontics 43, 1806–20.
Tsay RC, Vo J, Burke A, Eisig SB, Lu HH, Landesberg R (2005) Differential growth factor retention by platelet-rich plasma composites. Journal of Oral and Maxillofacial Surgery 63, 521–8.
Ulusoy A, Turedi I, Cimen M, Cehreli Z (2019) Evaluation of blood clot, platelet-rich plasma, platelet-rich fibrin, and platelet pellet as scaffolds in regenerative endodontic treatment: a prospective randomized trial. Journal of Endodontics 45, 560–6.


